What You Should Know:
A new report from the KLAS Arch Collaborative reveals that the overwhelming burden of documentation is a primary driver of nurse burnout, with 40% of nurses intending to leave the profession by 2029.
– The study also highlights that meaningful progress is possible: organizations that have implemented specific strategies to streamline charting—such as eliminating redundant fields and utilizing AI—have seen dramatic improvements in nurse satisfaction.
The Silent Crisis: Why Documentation Burden Is Driving Nurses Away and How Tech Can Bring Them Back
For years, nurses have served as the healthcare system’s “shock absorbers”. As regulatory requirements expanded and administrative tasks multiplied, nurses quietly adapted, absorbing the additional workload without complaint. But a new report from KLAS Arch Collaborative suggests that the shock absorbers are finally breaking.
The findings are stark: 40% of nurses intend to leave the profession by 2029. While salary and patient ratios are often cited as reasons for this exodus, the KLAS report identifies a pervasive, scalable, and fixable culprit: documentation burden.
“Highly adaptable nurses tend to persevere quietly with the additional burden, so their challenges often aren’t at the top of organizations’ priority lists,” the report notes. “But this is an industry-wide problem that needs to be addressed now.”
The Cost of “Unproductive Charting”
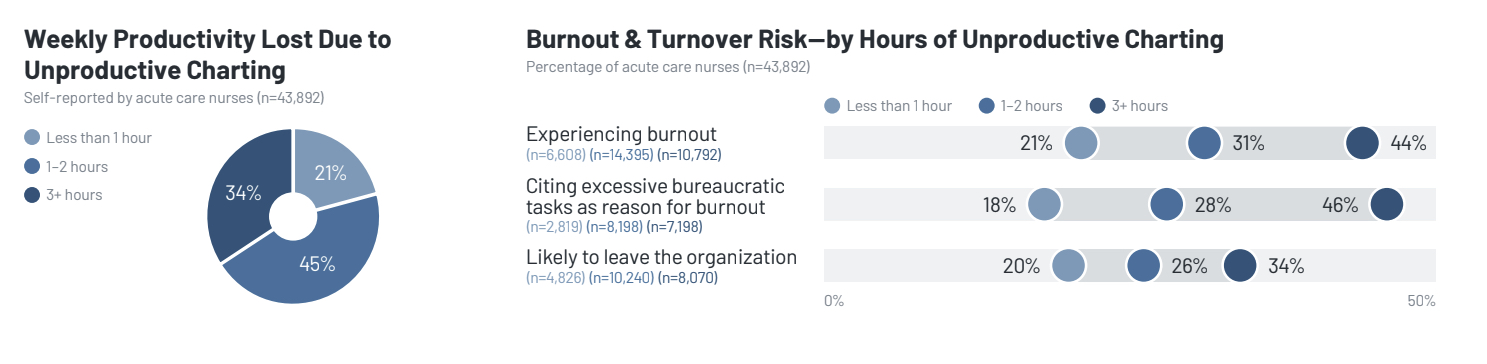
The report, based on data from over 80,000 acute care nurses, paints a picture of a workforce drowning in data entry. A staggering 79% of nurses report time lost to unproductive charting—defined as duplicative or unhelpful documentation.
The correlation between charting and burnout is undeniable. Nurses who spend 3+ hours per shift on unproductive charting report significantly higher rates of burnout (46%) compared to those who spend less than an hour (21%).
“It feels as though [we] are frequently forced to double chart and/or check two places for information, or important information will be missed,” one nurse respondent noted. “Then at the end, [we] are exhausted with very little to show for it.”
The top complaints from the front lines include:
- Duplicative Documentation: Cited by 60% of nurses, especially regarding flowsheets.
- Lack of Standardization: 26% of nurses are frustrated by inconsistent workflows for similar tasks.
- Excessive Fields: 16% report having to fill out fields that serve no clinical or regulatory purpose.
A Blueprint for Change
Despite the grim statistics, the report offers a roadmap for success. It highlights five organizations that have successfully turned the tide, achieving massive improvements in their Nurse Net EHR Experience Score (NEES).
Seattle Children’s Hospital, for example, achieved a 71.4-point improvement in nurse satisfaction—the largest increase seen in the collaborative. Their strategy? A two-year initiative focused on eliminating redundancy and leveraging data to identify high-impact optimization opportunities.
Wooster Community Hospital eliminated 96 documentation fields, saving over 15,000 nursing hours annually. Their “Freeing Up Nurses’ Time” initiative proved that removing clutter is just as powerful as adding new tools.
The Technology Fix
While workflow redesign is critical, the report emphasizes that technology is a key enabler. Several tools have been validated by KLAS to reduce burden:
- Mobile Documentation: Allows nurses to chart at the bedside, improving timeliness and accuracy.
- Device Integration: Automates data transfer from cardiac monitors and smart pumps, eliminating manual entry.
- AI Summarization: Generates concise patient summaries and end-of-shift notes, saving time on handoffs.
- Ambient Speech: An emerging technology that captures spoken observations and converts them into structured documentation.
