What You Should Know:
– According to Kaufman Hall’s 2025 Health System Performance Outlook, hospitals are facing a “financial trifecta” of rising non-labor expenses, workforce instability, and aggressive payer reimbursement pressures.
– Nearly 60% of health systems reported non-labor cost increases of up to 10%, driven by inflation and tariffs, while 44% cited high claim denial rates as a top challenge. As bad debt rises and staffing levels tighten, the report urges leaders to prioritize operational resilience and clinical integration to navigate the uncertainties of 2026.
The Resilience Mandate: Hospitals Battle Inflation and Denials as Margins Tighten
The financial recovery of the U.S. hospital system is hitting a new, complex wall. It’s no longer just about labor shortages; it’s about the rising cost of everything else, compounded by a reimbursement environment that is becoming increasingly hostile.
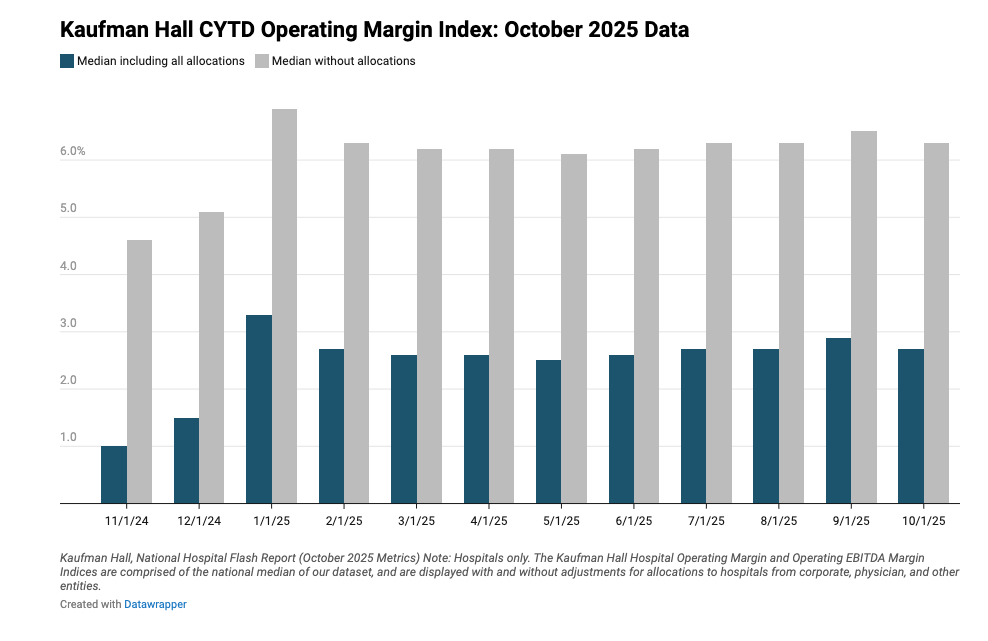
Kaufman Hall, a healthcare management consultancy, released its 2025 Health System Performance Outlook, painting a picture of an industry in a defensive crouch. Based on data from over 100 hospital leaders, the report identifies a convergence of pressures—non-labor inflation, workforce optimization struggles, and payer friction—that are threatening to erode the fragile margin gains of the past year.
The Non-Labor Inflation Spike
For the past two years, the narrative has been dominated by the cost of contract labor. Now, the ledger is flipping. Almost 60% of respondents reported non-labor expense increases between 6% and 10% over the past year.
This isn’t just standard inflation. Organizations pointed to specific external factors, including tariffs and supply chain disruptions, as leading drivers. In fact, 83% of respondents have already taken steps to quantify the specific impact of tariffs on their bottom line.
“While non-labor expenses are no doubt putting financial pressure on organizations, the 2025 findings may reflect broad inflationary pressure rather than abnormal spikes,” said Lance Robinson, Managing Director at Kaufman Hall.
The Workforce Paradox: Efficiency vs. Burnout
The report reveals a dangerous tension in hospital staffing. While hospitals are technically becoming more efficient, they may be running too lean. Data from the accompanying National Hospital Flash Report shows that the number of full-time employees (FTEs) is down, even as labor efficiency metrics rise. Erik Swanson, Managing Director of Data and Analytics, warns this is a red flag for “potential workforce burnout.”
To combat this, 70% of organizations are actively focused on workforce optimization. Strategies include:
- Wage Increases & Bonuses: Expanding signing and retention incentives to keep core staff.
- Advanced Practice Providers (APPs): 42% of respondents noted the value of APPs, though deployment remains highly variable, suggesting a missed opportunity for better clinical integration.
The Payer Battleground
Perhaps the most acute source of frustration for hospital executives is the behavior of payers. Forty-four percent of hospitals surveyed cited high denial rates and administrative burden as their top challenges with managed care organizations.
This friction is exacerbated by legislative uncertainty surrounding Medicaid. As bad debt and charity care continue to rise—a trend Swanson predicts will extend into 2026—hospitals are finding it harder to get paid for the care they deliver.
The volume is there—adjusted discharges are up 5% year-to-date—but the revenue per patient is slipping, down 3% month-over-month.
