What You Should Know:
– A new 50-state analysis reveals that over half (51.7%) of U.S. private-sector workers are now enrolled in high-deductible health plans (HDHPs) as employers struggle to manage rising costs. The report shows that annual family premiums jumped to $24,540 in 2024, outpacing inflation, while average family deductibles surpassed $4,000 for the first time.
– The trend exposes millions of Americans to greater financial risk in medical emergencies, signaling a deepening affordability crisis within the employer-sponsored insurance market.
Healthcare Affordability Crisis: 51% of Employees Pushed into High-Deductible Plans Amid Sharp Cost Hikes
For decades, the “gold standard” of American employment was the promise of robust health coverage. It was the bedrock of the social contract between the private sector and its workforce. Today, new data confirms that this foundation is cracking under the weight of unsustainable economics. A sweeping 50-state analysis released by the State Health Access Data Assistance Center (SHADAC) at the University of Minnesota paints a stark picture of the 2024 landscape. The primary finding is a tipping point: more than half (51.7%) of all private-sector workers are now enrolled in high-deductible health plans (HDHPs). This shift represents a fundamental transfer of financial risk from corporations to individuals, a gamble that researchers warn is becoming “increasingly unaffordable” for the 182 million Americans who rely on their jobs for coverage.
The Inflation Gap: Premiums and Deductibles Surge
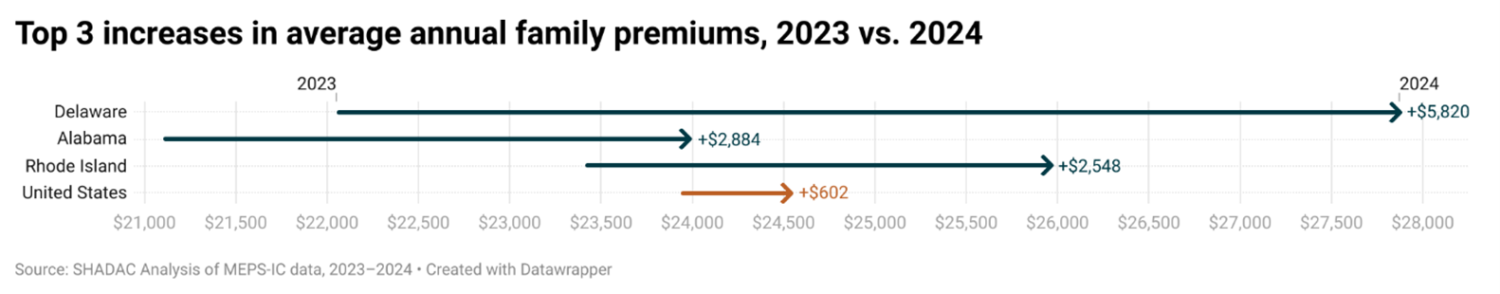
While the broader economy battled inflation in 2023 and 2024, healthcare costs didn’t just keep pace—they accelerated. According to the report, annual premiums for family coverage spiked to $24,540, a year-over-year increase of more than $600. Individual premiums followed suit, rising to $8,486. However, the sticker price of the premium is only half the story. The “hidden” cost of care—the deductible—grew even faster than premiums, rising an average of 8%.
For the first time in history, the average annual deductible for family coverage has surpassed the $4,000 mark. This means that before insurance kicks in for non-preventative care, families are on the hook for a sum that exceeds the total savings of many U.S. households.
“Employer-provided health coverage is not immune from the healthcare affordability crisis that is tightening its grip throughout America,” said Katherine Hempstead, senior policy adviser at the Robert Wood Johnson Foundation.
The High-Deductible Trap
The migration to HDHPs is understandable from a balance sheet perspective; employers move workers to these plans to shield them from even larger monthly premium hikes. However, this strategy is essentially a roll of the dice.
“It means greater financial risk down the road in the event of a medical emergency. It’s a gamble no one should have to take,” Hempstead noted.
The prevalence of these plans varies wildly by geography. The analysis indicates that in 22 states, enrollment in high-deductible plans now exceeds 60%. This disparity creates a fragmented landscape where the value of a “good job” differs significantly depending on where a worker lives.
Regional Volatility: The Delaware Anomaly
While the national trend is concerning, specific state-level data reveals pockets of extreme volatility. Delaware emerged as a startling outlier, seeing the largest increase in family premiums nationwide. Costs there surged by more than $5,800—a massive 26% increase taking premiums from $22,049 to $27,859 in a single year.
Alabama and Rhode Island also topped the list for significant year-over-year increases, highlighting that this is not solely a coastal or metropolitan issue, but a systemic one affecting diverse economies.
The Silent Crisis in Policy Debates
Despite Employer-Sponsored Insurance (ESI) covering 54.6% of the U.S. population, it remains curiously absent from major policy debates. Political discourse tends to focus on the Affordable Care Act (ACA), Medicare, and Medicaid.
Elizabeth Lukanen, director at SHADAC, argues this oversight is dangerous. “As policymakers look for solutions to curb the growing healthcare affordability crisis, addressing the decades-long trend of increasing costs in employer-sponsored insurance must be part of the conversation,” Lukanen stated.
The data backs this up: while private insurance coverage overall increased to 66.1% in 2024, ESI enrollment remained statistically flat. The growth in private coverage was driven by direct purchases and the Marketplace, suggesting that the traditional employer model has hit a saturation point or a ceiling of viability.
New Reality for Employer Sponsored Insurance
We are entering an era where having insurance and being able to afford healthcare are two increasingly distinct concepts. Unless policymakers and employers address the structural costs driving premiums and deductibles higher, the American workforce will continue to pay more for less.
