What You Should Know:
– A new, collaborative analysis conducted by the American Telemedicine Association (ATA) Center of Digital Excellence (CODE) and nine major U.S. health systems provides critical operational evidence on Medicare telehealth utilization patterns.
– The findings, based on real-world data across 1.67 million Medicare beneficiaries challenge traditional assumptions by demonstrating that virtual care is overwhelmingly substitutive—replacing, rather than adding to, existing care. The analysis examined operational data from nine health systems, including Advocate Health, Johns Hopkins Medicine, and UPMC, representing diverse models from academic medical centers to rural providers
Key Findings: High Substitution, Flat Utilization
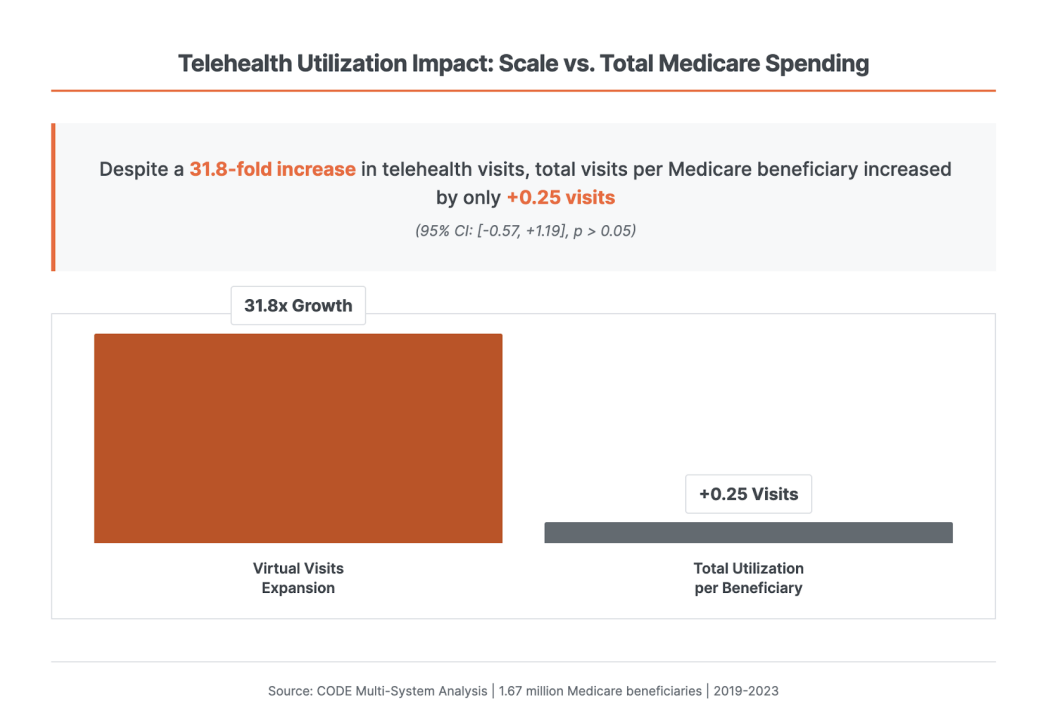
Despite a 31-fold increase in virtual visits across the participating systems, the total visits per Medicare beneficiary remained essentially unchanged, rising by only +0.25 visits per beneficiary on average
The key statistical finding is the substitution rate:
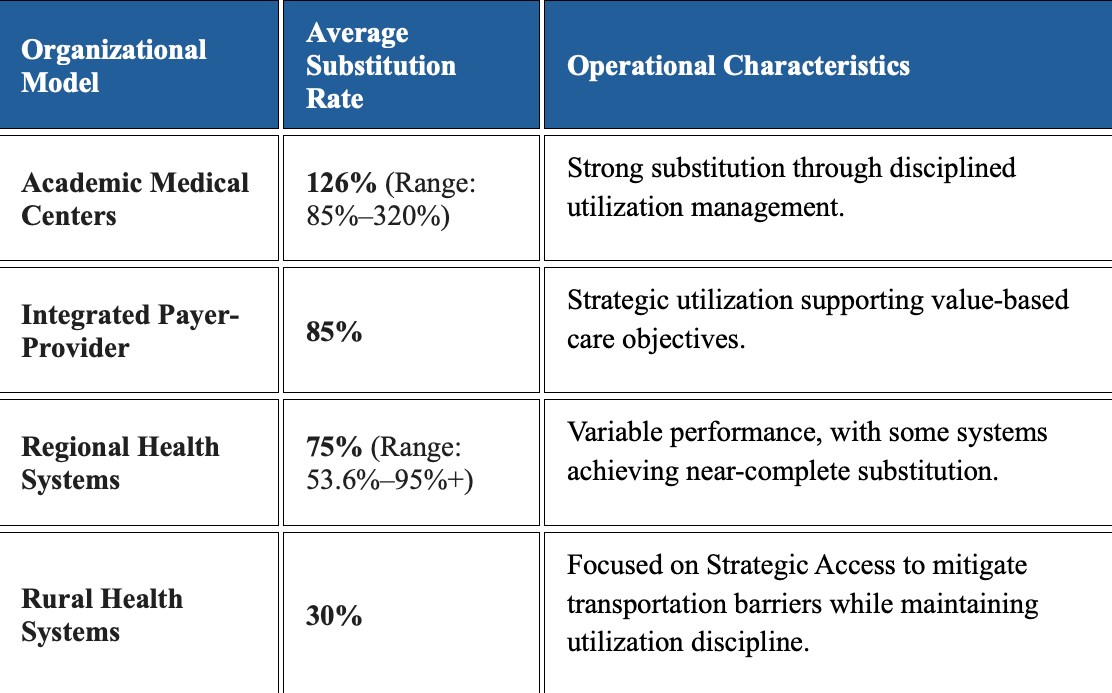
- Substitution Rate: Operational data suggests a population-weighted substitution rate of 74% (95% CI: [68%, 80%]) across participating systems
- Policy Relevance: This rate substantially exceeds the Congressional Budget Office’s (CBO) traditional assumptions of 30–50%
“Even with millions more virtual visits and the increased access to care, billed encounters per patient have stayed essentially flat,” said Ethan Booker, MD, FACEP, Chief Medical Officer for Telehealth at MedStar Health. In the largest Medicare population studied (over 350,000 beneficiaries), virtual visits grew by more than 200-fold, yet the total utilization increased by only +0.01 visits per patient.
Consistency Across Diverse Care Models
The analysis demonstrated that the substitutive patterns are durable and consistent across various healthcare delivery models and time periods (2022-2023 steady-state operations).
Cost and Workforce Benefits Confirmed
The operational evidence also points to significant benefits in cost and workforce sustainability:
- Cost Impact: Preliminary evidence indicates that costs remained stable or were reduced where measured. 70% of Medicare models demonstrated cost-neutral or cost-reducing patterns based on preliminary operational evidence.
- Rural Cost Savings: A rural health system case study validated these patterns by avoiding 2,551 patient transfers to tertiary care, resulting in $8.1 million in documented cost savings from avoided transfers and transport.
- Workforce Efficiency: One system documented 42,000 cognitive nursing hours saved through virtual observation technology, which helps relieve staffing shortages and improves clinician capacity. Furthermore, virtual roles offer flexible delivery options that systems report improved clinician retention.
Validation and Next Steps for Policy
This analysis provides directional operational evidence that stands apart from traditional claims-based studies by measuring clinical workflows and substitution patterns as they occur in practice. The findings give federal analysts a unique opportunity to see how telehealth is embedded in everyday care.
“This data represents current state under a patchwork policy environment,” said Elissa Baker, BSN, RN, project lead and founder of ATA CODE. “We’re just scratching the surface of what health systems could achieve with predictable legislative frameworks.”
