What You Should Know:
– Arcadia, a healthcare data platform, has announced the publication of its new research report, Scaling Smarter: The Data Strategies Powering High-Performing Health Plans. The report reveals a widening gap between the data capabilities that payers need and the tools, infrastructure, and analytics strategies that many still lack.
According to the report, a lack of a unified data foundation built around complete member 360 profiles can hinder the effectiveness of AI and other technologies, resulting in missed opportunities for savings and improved experiences. The report also highlights how leading health plans are making meaningful progress with data-driven strategies that improve outcomes, manage costs, and strengthen provider performance.
Data Integration Lags Behind Data Sharing
While many payers believe they have a complete picture of their members, the report suggests significant gaps exist in the data they are actually using. The report found that while 66% of payers rated their ability to share data externally as “very good” or “excellent,” only 57% said the same about integrating data from outside sources. In fact, 85% of payers have yet to integrate all available data into a centralized analytics platform, which limits their ability to generate comprehensive and actionable insights.
AI and Advanced Analytics Remain Untapped
The report highlights that AI and advanced analytics are largely an untapped opportunity for health plans. Less than 20% of plans use AI to develop care plans, summarize records, or drive member engagement. These are tools that could improve operational efficiency and accelerate performance gains.
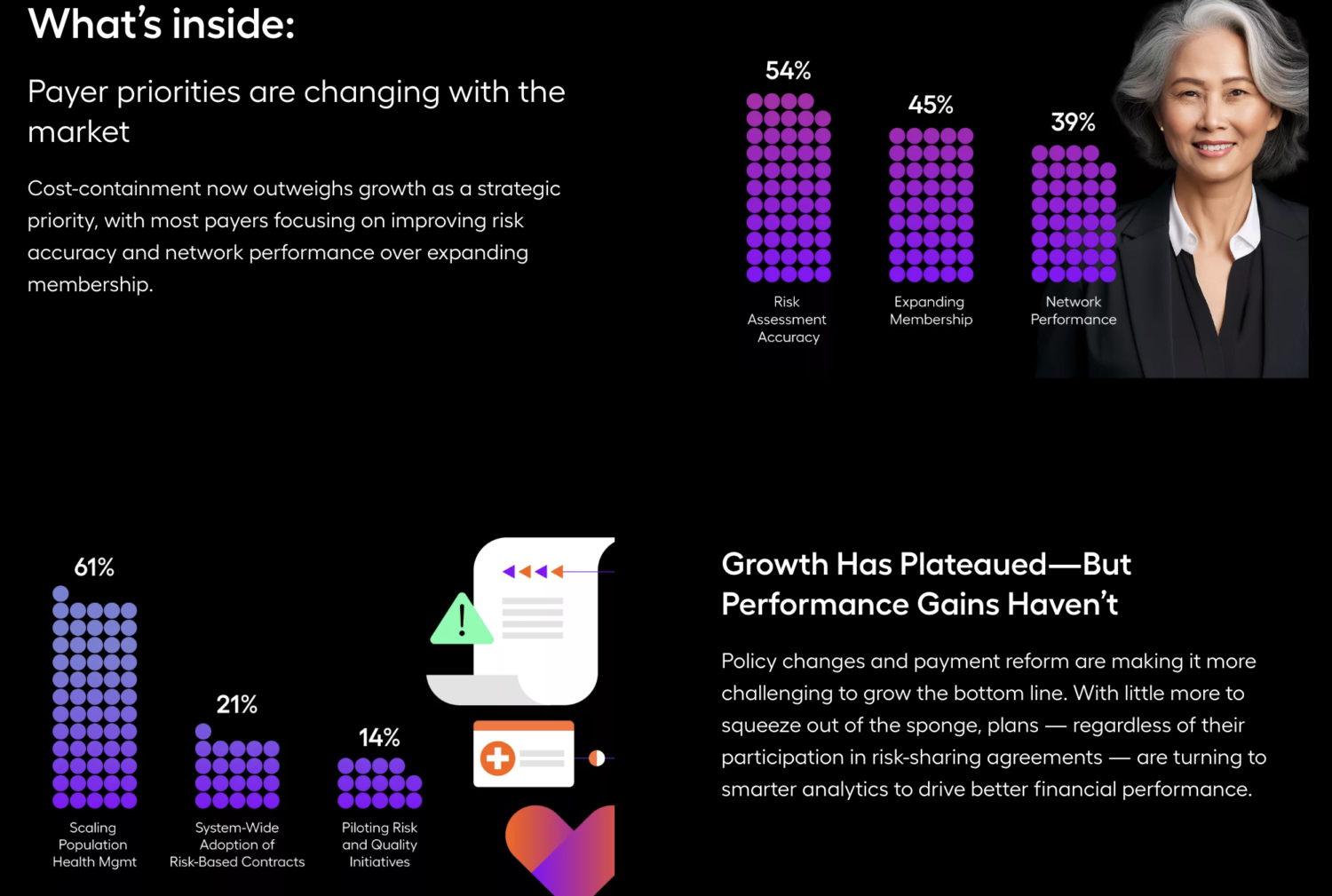
Additionally, the report found that cost pressures, such as improving risk adjustment (54%) and optimizing network performance (50%), are driving strategy more than revenue growth goals like expanding membership (45%).
Incomplete Member Profiles Create Missed Opportunities
While 96% of payers reported maintaining longitudinal member profiles, many admitted to facing challenges with data aggregation and interoperability. For instance, 76% of payers are not fully realizing the value of social determinants of health (SDoH) data, 87% are not using episode of care data, and only 10% are actively using pharmacy data. These missed opportunities can affect risk adjustment, personalized care, and cost efficiencies.“Too often, payers believe they have a complete picture of the member, but our research suggests there are significant gaps in what data they’re actually using—meaning missed opportunities to unlock better risk adjustment, personalized care, and cost efficiencies,” said Michael Meucci, President and CEO of Arcadia. “A true 360-degree member profile must include timely and complete information across claims, clinical encounters, SDoH, episodes of care, and pharmacy data. When payers integrate that data and apply it strategically, they can improve outcomes, reduce costs, and collaborate more effectively with providers.”
