What You Should Know:
– Innovaccer Inc., a healthcare AI company launches Flow Auth, a new AI-powered prior authorization solution.
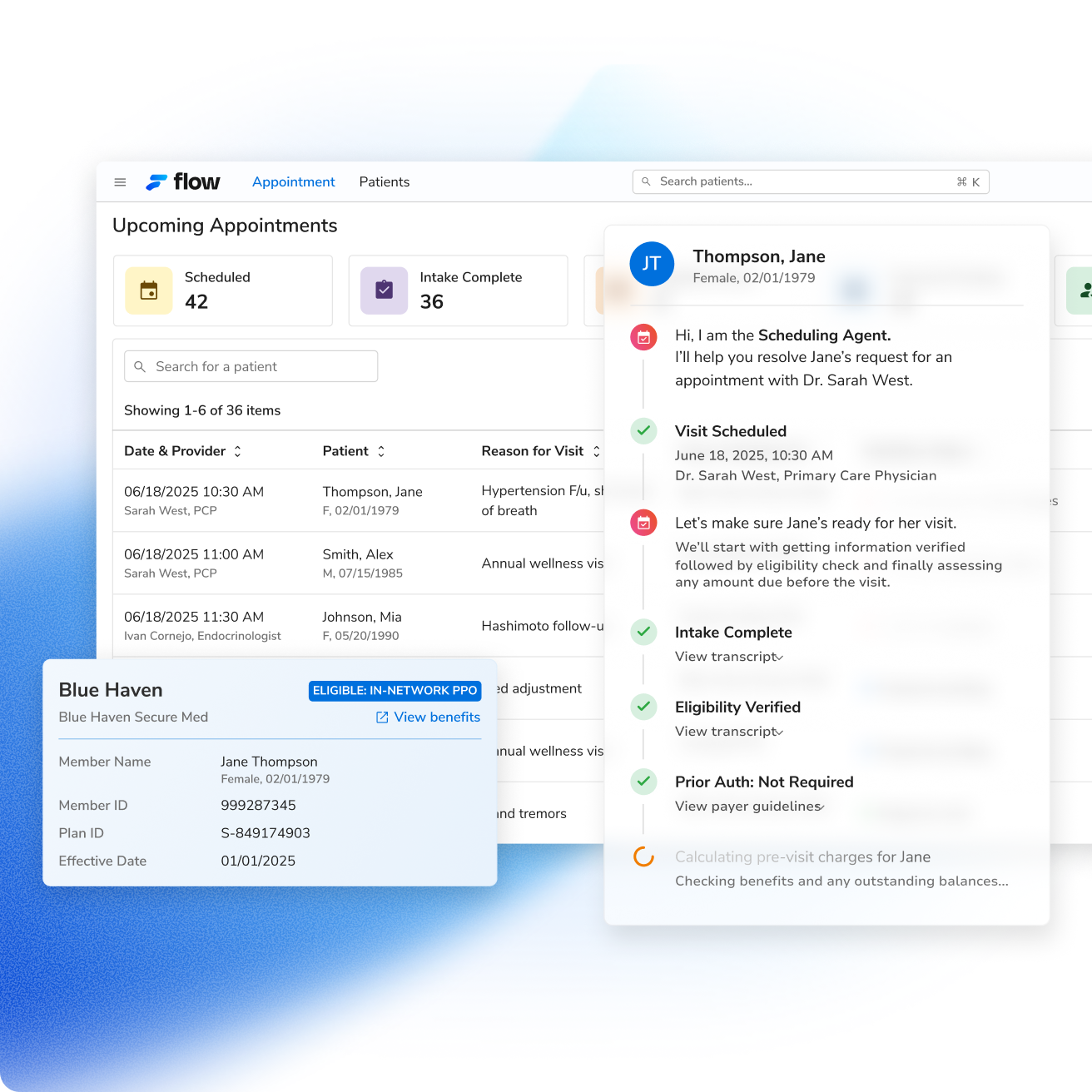
– As part of the company’s revenue cycle performance platform, Flow by Innovaccer, Flow Auth is designed to automate the entire prior authorization (PA) workflow, helping healthcare organizations accelerate care delivery and optimize revenue capture.
– Innovaccer projects that the solution could lead to a 50% reduction in the time clinicians spend on prior authorizations and a twofold increase in staff productivity.
Addressing the Buden of Prior Authorization
Prior authorization is a significant and widespread problem in healthcare. A 2024 survey by the AMA found that 94% of physicians believe prior authorization delays patient care, 27% report that requests are often or always denied, and 89% link the process to increased clinician burnout. Flow Auth directly addresses these challenges by automating the process from end to end, aiming to reduce delays, lower denial rates, and ease the administrative burden on clinical teams. This ensures submissions meet requirements on the first attempt, leading to faster approvals and reduced manual work.
Flow Auth Key Features
The platform includes several key features designed to streamline the prior authorization process:
- Proactive PA Detection: The system automatically identifies when prior authorization is required for an order based on payer-specific criteria within the EHR.
- Payer-Ready Packet Creation: It automatically gathers relevant clinical documentation, such as notes, labs, and imaging, flagging any missing items and organizing them in the format payers require.
- Full-Spectrum Submission: The solution can send packets using all available payer connectivity options, including APIs, portals, and fax.
- Real-Time Tracking: Flow Auth monitors the status of authorizations and provides updates within the clinical workflow.
- Automated Appeals Drafting: The system can help streamline appeals by drafting letters for denied requests, using historical outcomes and payer-specific policies to auto-fill necessary clinical details.
