What You Should Know:
– A newly released report from the Peterson Center on Healthcare offers critical guidance for policymakers navigating the rapidly expanding landscape of remote monitoring technologies.
– Synthesizing findings from three in-depth evaluations of digital health tools by the Peterson Health Technology Institute (PHTI) and analyzing trends in Medicare and Medicaid billing, the report sounds a timely alarm. It underscores the urgent need for a policy recalibration to ensure remote monitoring delivers genuine value to patients without escalating spending on ineffective or wasteful services.
– The report highlights the significant growth in both the number of patients utilizing remote monitoring services and the duration for which they are monitored. This expansion, coupled with the vast potential for further adoption, creates a pivotal moment for payers and policymakers to establish clear and effective guidelines. The core message is clear: coverage decisions must be driven by demonstrable value.
The Rapid Rise of Remote Monitoring and Its Fiscal Implications
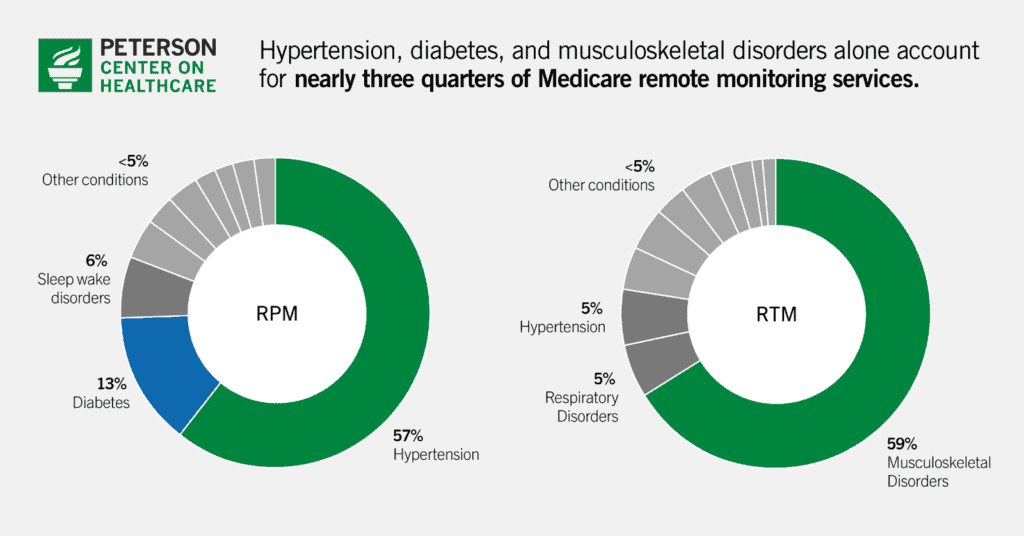
Remote monitoring, encompassing remote patient monitoring (RPM) for physiological data and remote therapeutic monitoring (RTM) for self-reported metrics, offers a promising avenue for managing patient health between traditional visits. However, the report reveals a concerning surge in Medicare billing for these services. Traditional Medicare spending on RPM skyrocketed from $6.8 million in 2019 to a staggering $194.5 million in 2023. Similarly, RTM, with codes introduced in 2022, witnessed a rapid increase from $2.2 million to $10.4 million in 2023 within traditional Medicare.
This exponential growth is particularly concerning given Medicare’s current payment structure, which offers the same reimbursement regardless of the condition being monitored and allows for indefinite billing periods. With a substantial portion of Medicare beneficiaries managing chronic conditions suitable for remote monitoring, the potential for unchecked spending is immense, demanding immediate policy attention grounded in evidence-based clinical benefits.
Key Recommendations for Policymakers and Payers
To ensure remote monitoring fulfills its potential as a valuable healthcare tool while mitigating the risk of wasteful expenditure, the Peterson Center report puts forth three key recommendations:
1. Let Performance Drive Coverage and Reimbursement
The report strongly advocates for a paradigm shift where coverage and reimbursement policies are firmly rooted in evidence-based research. Policymakers and payers should prioritize establishing whether, and for what duration, remote monitoring demonstrably improves patient outcomes for specific conditions. This necessitates a move away from blanket coverage and towards a more nuanced approach that recognizes the varying effectiveness of remote monitoring across different health conditions and monitoring durations.
2. Drive Access to and Use of High-Impact Services
To maximize the benefits of remote monitoring, the report recommends utilizing payment incentives to encourage the adoption of high-value services, particularly in underserved rural areas where access to traditional care may be limited. Conversely, policies should actively discourage the use of remote monitoring in situations where it offers little clinical benefit or contributes to wasteful spending. This targeted approach can ensure that remote monitoring resources are directed towards applications where they yield the greatest positive impact on patient health and healthcare efficiency.
3. Improve Data Collection and Transparency
A fundamental prerequisite for informed decision-making regarding the effective and efficient use of remote monitoring is the availability of comprehensive and transparent data. The report urges payers and policymakers to mandate the collection of more specific information about the implementation and outcomes of remote monitoring technologies. This includes details on the specific digital solutions employed, the types of physiological and other data being collected, the precise medical condition being managed, and relevant provider information. Enhanced data collection will empower stakeholders to conduct robust evaluations, identify best practices, and make evidence-based decisions about coverage and reimbursement.
Evidence from PHTI Evaluations and Billing Trends
The report’s recommendations are underpinned by PHTI evaluations of digital tools targeting diabetes, hypertension, and musculoskeletal disorders – conditions that account for a significant portion of current remote monitoring spending and utilization. In 2023, monitoring for diabetes and hypertension alone constituted 73% of total RPM spending in traditional Medicare, while musculoskeletal disorder monitoring represented the majority of RTM episodes and nearly half of RTM spending.
Furthermore, the analysis of billing trends reveals a concerning disconnect between clinical evidence and practice. For instance, while evidence suggests that remote patient monitoring for blood pressure management is most beneficial within the first six months, a substantial 40% of hypertensive Medicare beneficiaries were monitored for periods exceeding this timeframe. This highlights the need for policies that align reimbursement with the clinically demonstrated window of effectiveness.
“As we adopt exciting, new technologies that extend care beyond the walls of the doctor’s office, we need to design payment models that align with clinical benefits for patients,” said Caroline Pearson, executive director of the Peterson Center on Healthcare. “That means ending ‘forever codes’ that incentivize long-term billing of ineffective care and instead designing payments that reimburse providers for the periods of time they should be actively monitoring and managing their patients’ diseases.”
