What You Need to Know:
– LexisNexis Risk Solutions, that it has partnered with Clarify Health to evaluate the predictive capability of social determinants of health and clinical data.
– The collaboration’s approach will integrate individual-level SDOH data into Clarify Health’s clinical analytical models to evaluate the quality and efficacy of the data at the point of care to help drive care management decision-making.
– Clarify Health’s analytical models help identify population health gaps and opportunities for care delivery improvement and optimization by leveraging a holistic view of the patient and social risk factors.
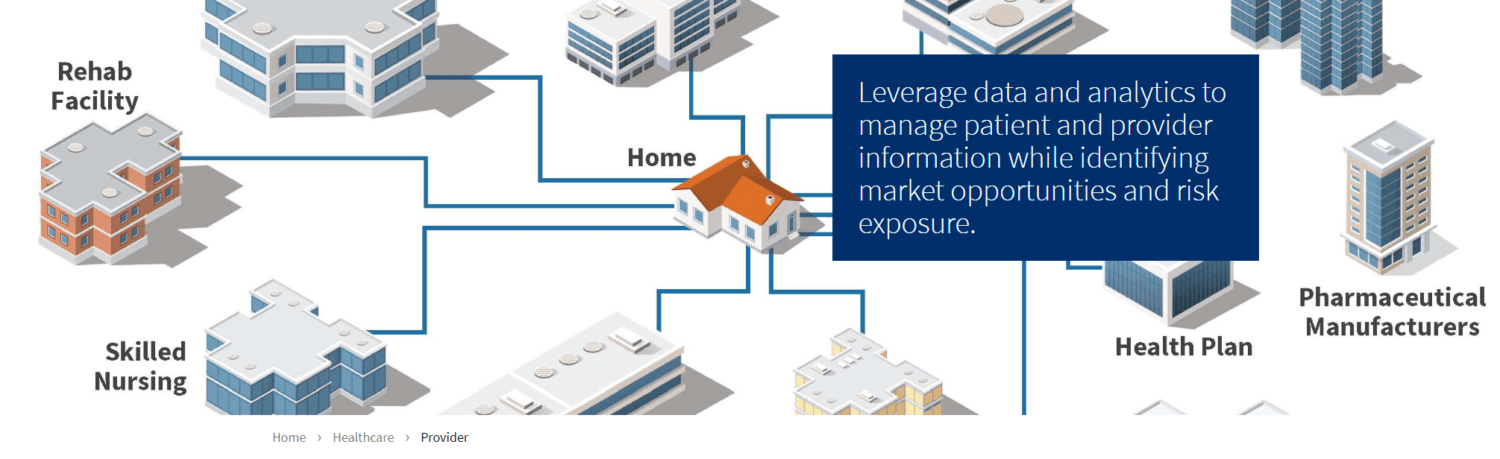
LexisNexis Risk Solutions announced a collaboration with Clarify Health, a healthcare analytics company that provides AI-driven market intelligence and predictive analytics business applications to health systems, health plans, and life sciences companies. The partnership will enable Clarify Health to use LexisNexis Risk Solutions socioeconomic data to better understand patient populations.
The goal is to leverage the LexisNexis Risk Solutions clinically validated social and behavioral determinants of health data, sometimes referred to as “SDOH” attributes, within predictive models that currently utilize clinical data to improve health outcomes, reduce costs and prevent readmissions.
For instance, clinically validated data attributes help predict the probability of a patient being readmitted to the hospital within 30 days. By evaluating each individual’s level of risk, providers can effectively prioritize resources for high-risk patients during discharge and follow-up care.
Incorporating SDOH data into clinical models to enhance predictive scores provides a more comprehensive approach to defining and understanding social and behavioral attributes, their impact and identifying interventions that may be most impactful for specific groups of patients.
Importance of Integrating SDOH Data into Clinical Models
Clarify Health’s analytical models help identify population health gaps and opportunities for care delivery improvement and optimization by leveraging a holistic view of the patient and social risk factors. For instance, clinically validated data attributes help predict the probability of a patient being readmitted to the hospital within 30 days.
By evaluating each individual’s level of risk, providers can effectively prioritize resources for high-risk patients during discharge and follow-up care. Incorporating SDOH data into clinical models to enhance predictive scores provides a more comprehensive approach to defining and understanding social and behavioral attributes, their impact and identifying interventions that may be most impactful for specific groups of patients.
Improving the Actionability of Insights
“Understanding the upstream and downstream impacts of social and behavioral determinants of health at both the population- and patient-level will improve the actionability of insights we generate. Partnering with LexisNexis Risk Solutions and pursuing research that better describes pathways between SDOH factors and health outcomes represents Clarify’s commitment to provider- and patient-centered healthcare. We are excited to be leading the way and establishing good practice around social and behavioral data integration in clinical models to improve patient outcomes and reduce healthcare-attributed costs,” said Hilary Placzek, senior director of research, Clarify Health.
“We know that socioeconomic factors have been shown to have a significant impact on our health,” said Todd Gottula, co-founder and chief product officer, Clarify Health. “By understanding a patient population outside of just a clinical perspective, you can enable actionable insights to enhance the delivery and quality of patient care. We chose to work with LexisNexis Risk Solutions because of the depth of their data insights and attributes that can help us identify gaps in care around healthcare utilization.”
