Change Healthcare’s new solution uses artificial intelligence and behavioral science to help Medicare Advantage plans precisely identify and increase chances for enrollment of dual-eligible members
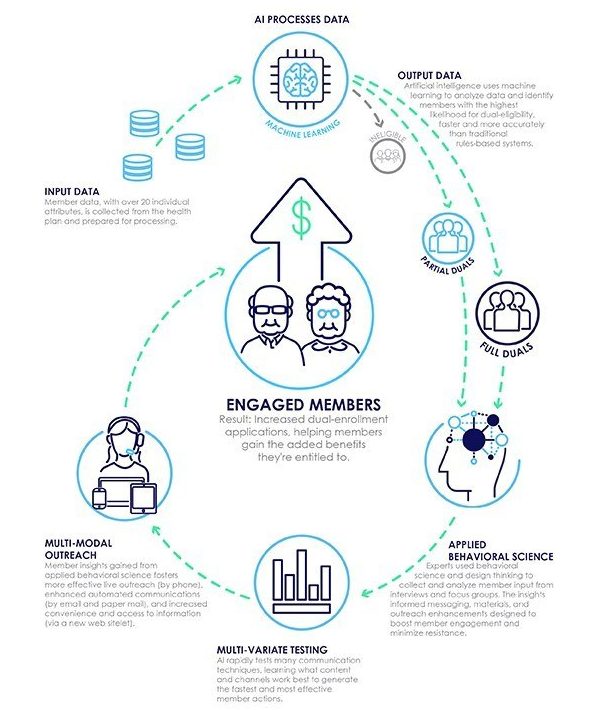
Change Healthcare, today unveiled Dual Enrollment Advocate, the first solution to blend artificial intelligence and behavioral science to help solve the challenge of Medicare Advantage (MA) dual-eligibility identification and enrollment. This new technology helps health plans more accurately identify, engage, and enroll MA members who are eligible for both Medicare and Medicaid.
There are 58.5 million Medicare beneficiaries today1, and 34% of them live at or below the Federal Poverty Level2, indicating many might be eligible for Medicaid. Meanwhile, only about 10.6 million of 19 million Medicare Advantage members are dual-enrolled, representing a significant opportunity for Medicare Advantage plans.3 The Change Healthcare Dual Enrollment Advocate uses AI to pinpoint, with up to 93%* accuracy, those individuals with the highest likelihood to qualify for full or partial dual eligibility. The result is that Medicare Advantage plans can quickly engage with this population and potentially enroll more of them faster.
Health plans traditionally have identified dual-eligible candidates using systems that require manual programming, continual updating, and are limited by small data sets and legacy technology. Dual Enrollment Advocate enables the rapid analysis of massive amounts of data in a fraction of the time otherwise required to identify optimal targets’ dual-eligible status.
This proprietary AI technology is deployed in concert with Change Healthcare member engagement teams, which apply behavioral science that uses intelligence gathered through consumer and expert interviews, focus groups, in-home immersions, and by engaging with beneficiaries. The engagement teams use Member Advocates, targeted mailings, and other outreach methods to more effectively activate dual-eligible members and support them through the enrollment process.
“We’re applying data science, behavioral science, and consumer-experience design to solve one of the trickiest problems for Medicare Advantage plans, which is how to accurately identify people for Medicaid eligibility,” said Keith Roberts, vice president, Engagement, Change Healthcare. “AI and machine learning can’t do it alone. Behavioral science can’t do it alone. And health plans and legacy systems can’t do it alone. The time has come to bring these healthcare IT and scientific disciplines together to help solve a critical business challenge for our customers.”
