Surescripts, a health information network, is expanding to support population health management with its Medication History for Panel Management service for health systems, accountable care organizations (ACOs) and analytics vendors.
The service, Medication History for Panel Management Service, comes at a time when managing population health is a top priority for care providers, especially in light of value-based payment models.
Key features of the service include:
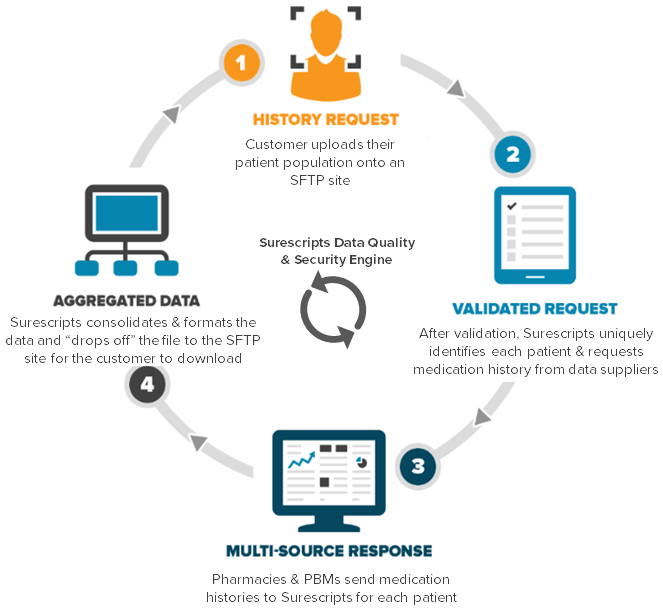
· Delivers fresh, accurate medication history information for a care providers’ entire patient population at one time via a single connection to 14 nationwide pharmacies with 28,000 store locations and two pharmacy benefit managers.
· Gives healthcare providers access to more holistic, standardized and timely medication data, allowing them to better manage the quality of care across large patient populations.
· Unlocks access to updated, multi-sourced medication information that is monitored and reviewed for quality—a game-changer for improving population health capabilities.
· Helps providers adjust to new performance-based payment reforms that are replacing volume-based measures with incentives to promote safer and more effective patient outcomes.
Comprehensive patient medication data is essential to using population health analysis to improve patient care, reduce admissions and readmissions and manage costs, but getting this data is still a challenge for hospitals, health systems and ACOs. Surescripts’ Medication History for Panel Management Service is working to fix this gap.
“With the shift to value-based reimbursement models, every provider across the healthcare system needs better information to effectively manage the health of patient populations,” said Tom Skelton, Chief Executive Officer of Surescripts. “Our panel management service provides the market’s most complete view of patients’ medication information, allowing greater visibility into their overall health, and ultimately improving the quality of care for patients nationwide.”
Surescripts Medication History for Panel Management helps providers adjust to new performance-based payment reforms that are replacing volume-based measures with incentives to promote safer and more effective patient outcomes. This service is designed to meet the demands of the Medicare Access & CHIP Reauthorization Act (MACRA) which will govern reimbursement for all office-based treatment of Medicare patients, including the Advancing Care Initiative that aims to incentivize improvements in information to guide better decision-making by providers.
