The cost of following-up on late insurance claims is significantly higher than most industry estimates, according to new survey from Recondo Technology. The survey reveals that despite the availability of exception-based processing to automate the resource-intensive claim follow-up process, most hospitals rely on legacy outsourced or employed manual approaches that have generally failed to lower costs.
Survey Background
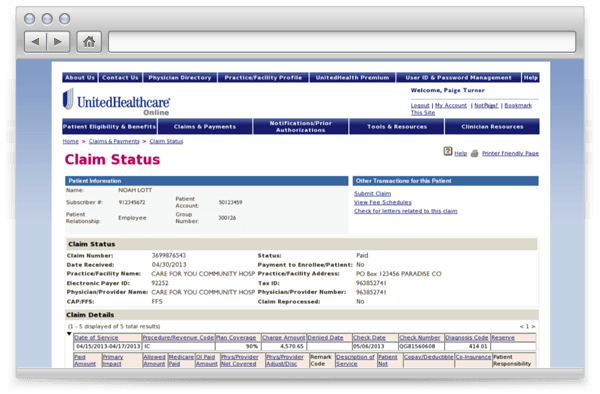
Recondo surveyed 80 healthcare finance professionals from hospitals, physician groups and consultant organizations in November 2015 during a Recondo-sponsored Healthcare Financial Management Association (HFMA). Respondents provided a high-level view of the current state of medical claims follow-up – the process by which hospitals and physician groups query insurers about the disposition of bills submitted for patient services. Claim follow-up is traditionally done over the phone by back-office staff, who can review no more three or four claims at a time, depending on the payer’s rules.
