Healthcare Exchanges have brought a new level of complexity to the payer and employer benefits landscape. Just how do plans retain employers and attract individuals while managing the risk pool?
With the advent of ACA, healthcare exchanges and various trends towards consumerism in healthcare, the health insurers are looking for ways to sustain their business in what could be a competitive marketplace. And also there is a need for them to directly market and sell the value of their services to individuals to differentiate.
The goals are to sustain the business, preserve the reserves, maintain profitability. The way to attain the goals are to manage the risk pool. In order to manage the risk pool, they have to attract right risk from exchanges, retain their existing good risk and manage the poor risk. The strategies to do this include:
o Direct Marketing, communication and targeting the consumers in the right geographies
o Devising products for the consumers and small groups, that attract the right segments – and include incentives and disincentives.
o Analyzing the current customer base to figure out which small groups might be vulnerable for moving to exchanges.
One of the key factors to determine the risk is to understand the health and behavioral factors of the consumer and how they will behave in the future with respect to utilization of health services and also compliant with medications, preventive screenings, etc.
Consumer segmentation is a key technique that is increasingly useful for understanding the individual and small group consumer pool to devise marketing and product packaging strategies to attract the right risk and to retain and manage risk.
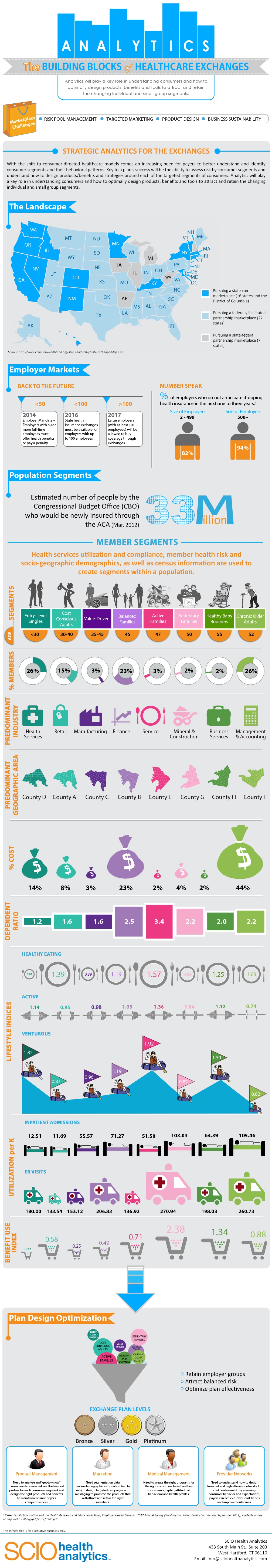
This infographic shown below created by SCIO Health Analytics illustrates the evolving medical benefit landscape and the importance of consumer segmentation for designing plans and strategies via:
- Exchange Landscape
- Employer Markets
- Population Segments
- Plan Design Optimization
SCIO Health Analytics helps payers, employers and PBMs solve significant business problems through actionable analytics and payment integrity solutions that are supported by extensive industry expertise and cutting-edge technology. SCIO provides both flexible and scalable analytics resources and solutions to meet the specific needs of their clients. They helps clients qualify plan designs and care programs that improve healthy outcomes and reduce costs.
