What You Should Know:
- Pear Suite, a digital health company dedicated to empowering community health workers (CHWs), today announced it has closed a $7.6 million Series A funding round co-led by Rock Health Capital and Nexxus Holdings.
- The investment will accelerate the development of its AI-powered platform, fuel provider network growth, and expand its impact through new Medicaid and Medicare health plan contracts.
Building Sustainable Infrastructure for Community-Based
Read More
Artificial Intelligence in Healthcare | News, Analysis, Insights - HIT Consultant
UnityAI and Peregrine Health Launch ‘Emma’ to Scale Behavioral Care in Underserved Communities
What You Should Know:
- UnityAI, a leading agentic AI company, has announced an exclusive partnership with Peregrine Health, a tech-enabled behavioral health company serving underserved communities through Federally Qualified Health Centers (FQHCs).
- The collaboration has successfully delivered and deployed Emma, a virtual care navigator that leverages UnityAI’s technology to modernize and scale patient engagement across behavioral health services.
Emma: A Virtual Navigator
Read More
Cleveland Clinic Deploys GenAI for Coding and CDI Across Enterprise Powered by AKASA
What You Should Know:
- Cleveland Clinic, one of the top academic medical centers in the U.S., has significantly expanded its partnership with AKASA, a leader in healthcare AI, to deploy an advanced Clinical Documentation Integrity (CDI) solution across all of its U.S. locations.
- The enterprise deployment follows a successful pilot and the system-wide adoption of AKASA’s AI coding tool, solidifying Cleveland Clinic’s position as a pioneer in applying generative AI (GenAI) to
Read More
Agentic AI in Healthcare: Hype or Healthcare’s Best Co-Pilot?
“AI is going to replace doctors.”
It’s a provocative, yet increasingly common fear whispered in hospital corridors and debated in medical forums. For many clinicians, the idea that software could not only analyze data but in the case of Agentic AI, take action evokes a dystopian future of medical decision-making stripped of empathy, nuance and professional judgment.
But fear, in many cases, is a symptom of misunderstanding. And for Agentic AI,
Read More
AGS Health Unveils Agentic AI Solutions to Combat Rising Claim Denials and Margin Pressure
What You Should Know:
- AGS Health®, a strategic growth partner and leading provider of tech-enabled RCM solutions, today announced the introduction of a new suite of agentic digital workforce solutions.
- Powered by AI agents and intelligent automation, these solutions are designed to help healthcare providers navigate the unprecedented strain caused by rising claim denials, severe staffing shortages, and mounting financial pressures.
Market Pressures Driving Urgent Change
The
Read More
Marc and Lynne Benioff, Salesforce Donate $100M to UCSF Children’s Hospitals
What You Should Know:
- Marc and Lynne Benioff, alongside Salesforce, an AI CRM, today announced a massive philanthropic commitment to the Bay Area community.
- The Benioffs are donating $100M to UCSF Benioff Children’s Hospitals to expand and modernize pediatric care. This gift is part of a combined $139 million in new support from the Benioffs and Salesforce, pushing their total community contributions in the Bay Area past the $1 billion mark.
Deep-Rooted Commitment to
Read More
Infinx Invests in Voxology AI: Voice-First Automation Transforms Patient Access and Revenue
What You Should Know:
- Infinx, a prominent provider of AI-powered solutions for patient access and revenue cycle management (RCM), announced a strategic investment in Voxology AI, a healthcare technology company specializing in conversational AI agents for the front office.
- The partnership integrates voice-first automation directly into Infinx’s contact center solutions, creating a unified platform that manages both patient-facing front-office workflows and back-office
Read More
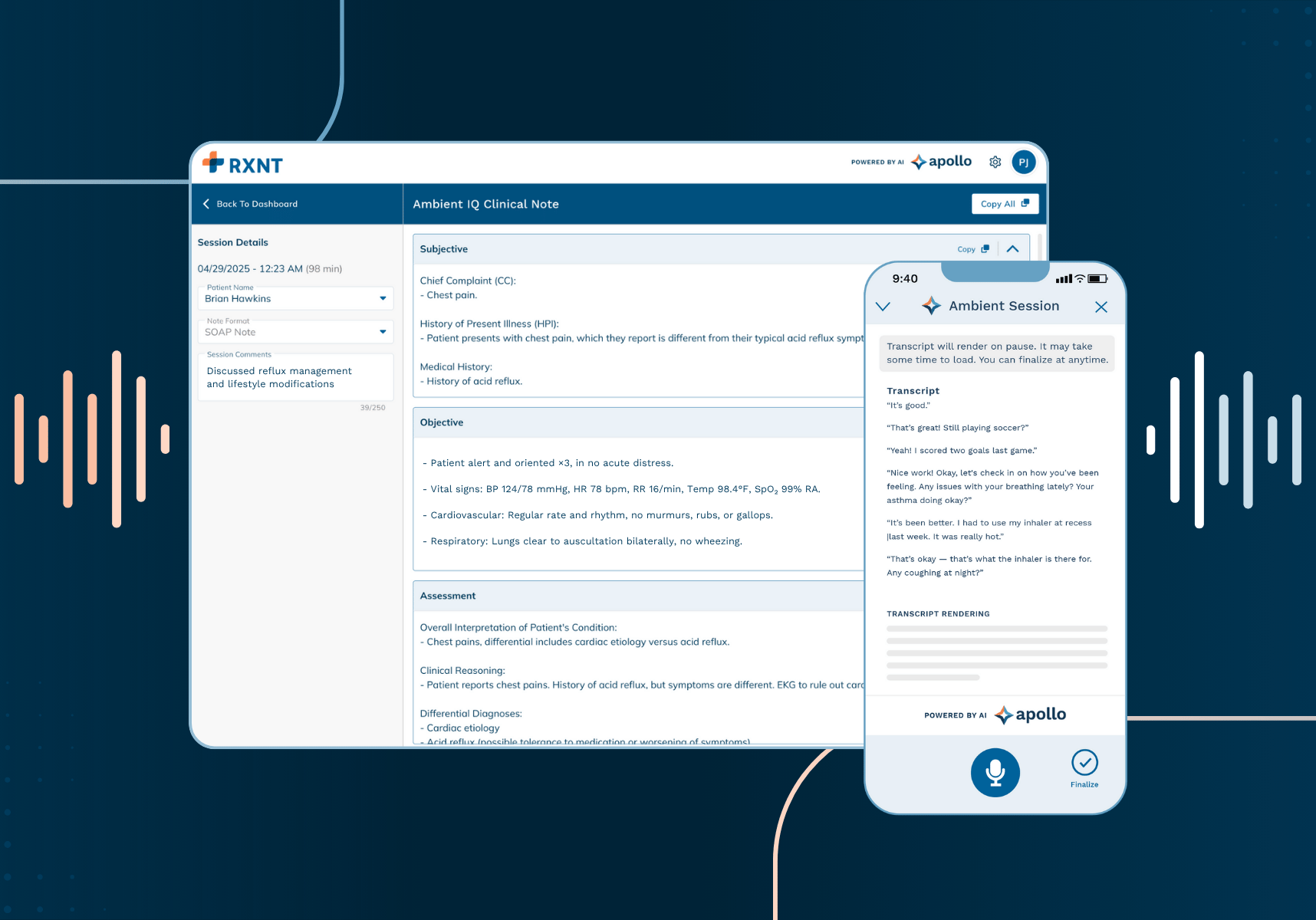
RXNT Launches Ambient IQ: AI Documentation Tool Cuts Provider Time by 70% for Just $75/Month
What You Should Know
- RXNT, a Maryland-based ambulatory healthcare technology pioneer, has announced the upcoming launch of Ambient IQ, an AI-powered ambient listening, transcription, and documentation tool.
- Ambient IQ will be available standalone for any provider in the United States starting in early November. This solution directly addresses the widespread issue of physician burnout, which is often driven by excessive documentation.
A Game-Changer for Provider
Read More
Olympia Orthopaedic to Deploy Innovaccer’s AI AGents for Automated Referral and Scheduling Workflows
What You Should Know:
- Innovaccer Inc., a healthcare AI company, has announced a new partnership with Olympia Orthopaedic Associates (OlyOrtho), a full-service musculoskeletal care provider in Southwest Washington.
- The collaboration focuses on using AI-powered tools to automate OlyOrtho’s referral and scheduling operations, enabling the independent practice to scale access, improve throughput, and reduce manual administrative work.
AI Agents Tackle Front-Office
Read More
AVIA Launches Nexus Agentic AI Collaborative to Combat High AI Project Cancellation Rates
What You Should Know:
- AVIA has launched Nexus Agentic AI, a new platform designed to help health systems responsibly adopt Agentic AI. The launch addresses a significant industry risk: more than 40% of Agentic AI projects are expected to be canceled by 2027 due to escalating costs, unclear business value, or inadequate risk controls.
- The new Nexus Collaborative aims to empower health systems to reshape operations, strengthen the workforce, and improve patient access and
Read More