My grim (and not-so-bold) prediction for the year ahead: Cost challenges will dominate leadership meetings throughout the year. My recommendation: Don’t let cost reduction be the only response. Instead, consider how building social capital can help organizations improve efficiency while also improving quality.
The financial pressures on organizations throughout healthcare are already intense, and only likely to worsen. Many providers and payers are running financial deficits, and no one feels like their business model is secure. Costs and utilization of healthcare are rising, and both government and employers are trying to keep their increases for spending on healthcare at the rate of inflation. Regardless of whether planned Federal cuts in healthcare spending occur in 2026, the pressures to do more with less are likely to be relentless.
Every organization will need to apply short-term tactics to reduce their costs and provide more care to more patients with the same infrastructure. But cost-cutting and working harder are tactics for the short-term, not a replacement for medium- and long-term strategies. Organizations need to do more than try to survive; they want to thrive. And to do that, they have to be ready to redesign care, to apply AI, and to build social capital.
It’s much easier to talk about the need to redesign care than to actually do it, and it’s much easier to get excited about the promise of AI than to improve efficiency through its use. Nevertheless, I’m optimistic that we’ll make real progress in both in the year(s) ahead for a simple reason – we have no choice.
The gap between patients’ needs and available personnel is growing, and either patients will not receive care that they need/want, or we will have to figure out new ways to care for them besides the in-person doctor visit. New models that use AI, virtual care, and non-physicians are sure to emerge as options that provide rapid access and possibly reduce costs.
How should these new models be designed? The goal should be improving value. The phrase “value-based care” was introduced only two decades ago (by my colleague Michael Porter), and there is a common misconception that value-based care means a change in the payment system whereby providers who spend less money in the care of their patients can share in the savings. The actual focus of value-based care is improving patient outcomes – and then turning to the work of making care as efficient as possible.
The mechanism for improving value (outcomes and efficiency) is integration of care. To develop these new models and spread them effectively and rapidly, organizations should emphasize some key social capital themes:
- Horizontal “bridging” connections – Managers/leaders need relationships through which they learn from colleagues doing the same work they do elsewhere within or outside their organizations. They need to build these relationships now so that they can trust what they learn from others tomorrow. It’s one thing to say we should all be ready to learn from others and spread innovations rapidly; it’s another to create the networks of relationships that accelerate those critical steps.
- Adjacent “bridging” connections – Managers/leaders should ask themselves two questions: Who uses my work? And whose work do I use? Then they should have direct conversations with their “suppliers” and “customers” to see how they create efficiency and improve effectiveness through more effective collaboration. This type of social capital building enlarges the idea of “we” among people on teams in healthcare. There is every reason to believe that patients appreciate the teamwork that results, and employees do as well.
- Vertical “bridging” connections –– also known as alignment. The people working at the front lines of healthcare organizations need to be able to trust that senior leadership shares their values and has good plans that reflect those values. That means that managers need to support communication between the C-suite and the front lines, and they should never “throw the C-suite under the bus” in order to cultivate stronger relationships with their reports.
- “Bonding” connections within teams. As new models that potentially improve efficiency are proposed, teams need the psychological safety that enables employees to speak up if the changes threaten safety or create harm in other ways. And the team culture needs to support behavioral norms that make implementation of the new models more effective.
The good news is that building social capital through these steps improves performance of all types. It improves safety, quality, patient experience and employee retention. It’s time to put social capital to work improving efficiency as well. The times that lie ahead are likely to reward the organizations that can.
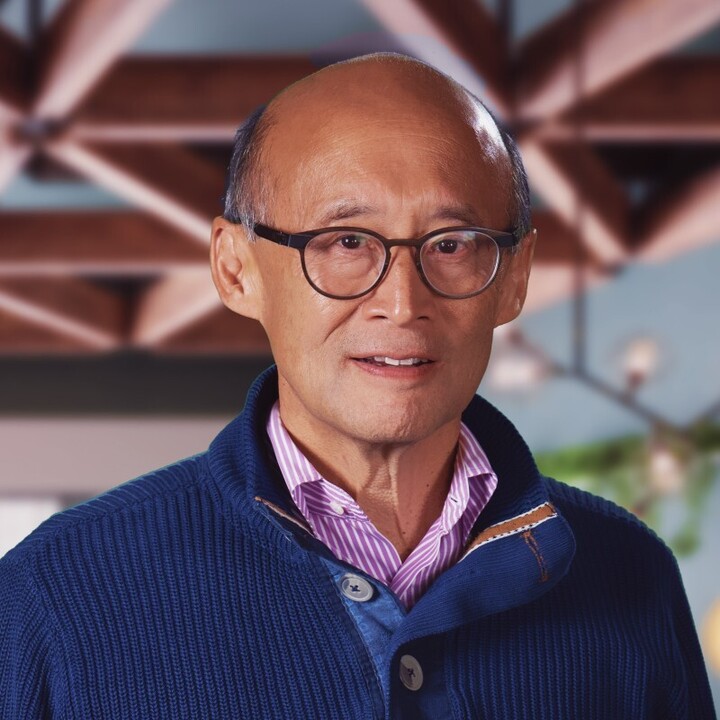
About Dr. Thomas Lee
Now the Chief Medical Officer at Press Ganey, Dr. Thomas Lee has more than three decades of experience in healthcare performance improvement as a practicing physician, a leader in provider organizations, a researcher, and a health policy expert. He recently published ‘Social Capital in Healthcare’, where he describes a new and powerful framework for improving healthcare, arguing that managers should approach the work of building trust, teamwork, and high reliability with the same intensity and discipline as CFOs use when managing the finances of their organizations
