What You Should Know:
– Medallion, a provider of AI-powered provider network infrastructure, today announced it has raised $43M in new funding led by Acrew Capital, with participation from Washington Harbour Partners and returning investors including Sequoia Capital, GV, and Spark Capital. The funding brings the company’s total raised to $130M, reinforcing its mission to eliminate administrative waste and streamline healthcare operations.
– The company plans to automate thousands of state-, provider-, and payer-specific workflows. In addition to scaling its technology, Medallion will invest in its go-to-market teams and strategic partnerships to accelerate growth across health systems, provider groups, and health plans.
Introducing CredAlliance: A Shared Credentialing Solution
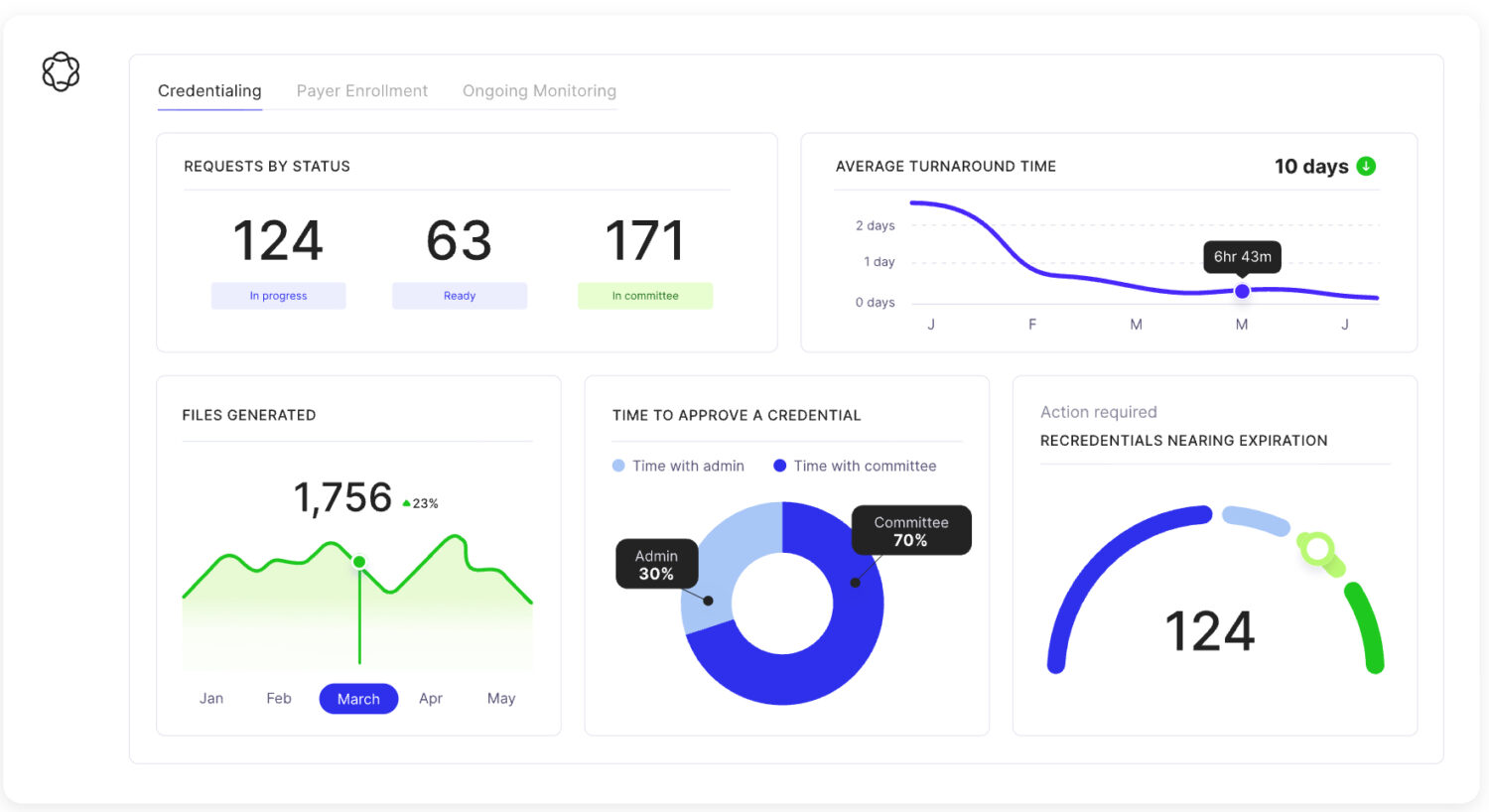
Medallion’s platform uses intelligent automation to replace repetitive, manual workflows in the healthcare back-office, tackling key challenges like credentialing, enrollment, onboarding, and compliance. The company’s technology serves as a unified system of record for provider data, helping health organizations and plans connect patients with providers more efficiently.
A core focus of the new funding is the public launch of CredAlliance, which Medallion bills as the industry’s first shared credentialing infrastructure for payers. This new service directly addresses a massive pain point in the healthcare system: the duplicative effort of each health plan independently re-credentialing the same providers. This process is estimated to cost the system $1.2B annually.
With CredAlliance, providers are verified once, and the results are syndicated across participating payer networks. This not only reduces costs but also allows providers to become billable across networks much faster, ultimately improving patient access and continuity of care. The platform is already live with several major national payers and is seeing strong demand from others to join.
Recent Traction/Milestones
Medallion’s funding round comes after a period of remarkable growth. The company has demonstrated a clear impact on efficiency, with key achievements including:
- 40x faster provider onboarding, reducing intake time from 8 days to under 2 hours.
- The introduction of advanced automations, such as AI phone agents and tools that map web forms to its data model without human intervention.
- A 106% increase in enterprise Annual Recurring Revenue (ARR).
- The launch of three new products: Privileging, Integration Engine, and CAQH Management.
Today, Medallion’s platform supports approximately 1 million providers, or about 10% of the U.S. healthcare workforce. By streamlining these crucial back-office functions, Medallion helps healthcare organizations eliminate hundreds of thousands of hours in administrative burden each year and has supported access to care for an estimated 240 million patients nationwide.
