
Sempre Health, a solution for advancing behavior-based pricing reductions for medication adherence, and UPMC Health Plan, which is part of UPMC, the second largest integrated health system in the U.S., today announced an expanded collaboration to improve affordability and adherence for critical medications. Starting this week, Sempre Health and UPMC Health Plan will now make additional medications available to even more members and products lines to impact members’ outcomes.
Prevalence of Cost-related Non-adherence to Medications
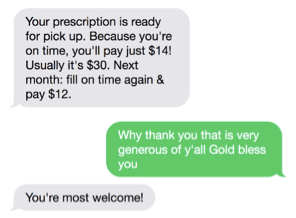
Nearly one-third of patients skip or delay filling prescriptions or taking medication because of cost. The prevalence of cost-related non-adherence to medications can dramatically affect health outcomes and is even higher following a significant medical event, such as a heart attack. Since 2017, Sempre Health applied innovative technology to send text message reminders to UPMC Health Plan members who were taking a key cardiovascular drug. When members filled their prescriptions on time, they paid less for the medication. Early results reveal that this pioneering discount model resulted in significant improvement in member engagement and increased adherence to the medication over 12 months.
Program Early Success
Over the first year of the collaboration, the program successfully enrolled more than one-in-three eligible members and led to significant improvements in adherence versus a control group. Additionally, the natural language text reminders and conversations with members led to increased engagement by creating a personalized and concierge experience for those enrolled.
Members reported increased affordability and satisfaction. Among the feedback from members are comments such as, “I like saving the money and being reminded to pick my meds up on time. I don’t see a downside.” Another member commented, “I like that I get reminded and that it gets cheaper when I refill on time.”
An example of a text reminder delivered by Sempre Health and received by a UPMC Health Plan member.
“Our growing partnership with UPMC Health Plan enables patients across Pennsylvania to share in the savings they generate when they are responsible with their health,” said Anurati Mathur, CEO of Sempre Health. “We’re excited to build upon our strong outcomes to date and further improve medication affordability and access for the members who need us most.”
