
AbedGraham of Healthcare Strategies’ Dr. Saif Abed talks why Clinician as a Service (ClaaS) model is a game changer for the industry when it comes to developing and implementing successful HIT.
While many tech developers gather around whiteboards and meeting tables to tackle healthcare’s challenges by exploring the latest in technical specs, there is often something missing amongst all the chatter regarding APIs, the newest software, and algorithms—human expertise.
According to Dr. Saif F Abed, founding partner of AbedGraham Healthcare Strategies, we aren’t talking about just conventional industry wisdom. Whether it’s tech developers creating the latest innovations, or healthcare organizations attempting to implement and integrate new technologies, clinical expertise has long been lacking as a part of the process, so much so, that the business of leveraging it has become AbedGraham’s focus since the company started in 2011.
“What we didn’t realize, was how sorely suppliers need precisely that kind of expertise. Too often sales and even deployments were stalling because clinicians didn’t feel products met their requirements and despised the fact that they hadn’t been consulted, said Abed. “IT was being done ‘at’ them rather than with them, and frankly, we knew where they were coming from exactly.”
Realizing what was missing was vital to the success of HIT’s evolution, Abed founded AbedGraham with fellow physician Alexander Graham fueled by the belief that one of their most valuable assets was their clinical experience. As a result, AbedGraham has made it a core objective to work with suppliers that recognize the challenge and to provide them with the clinical know-how and capabilities to become more clinically credible, relevant, and savvy.
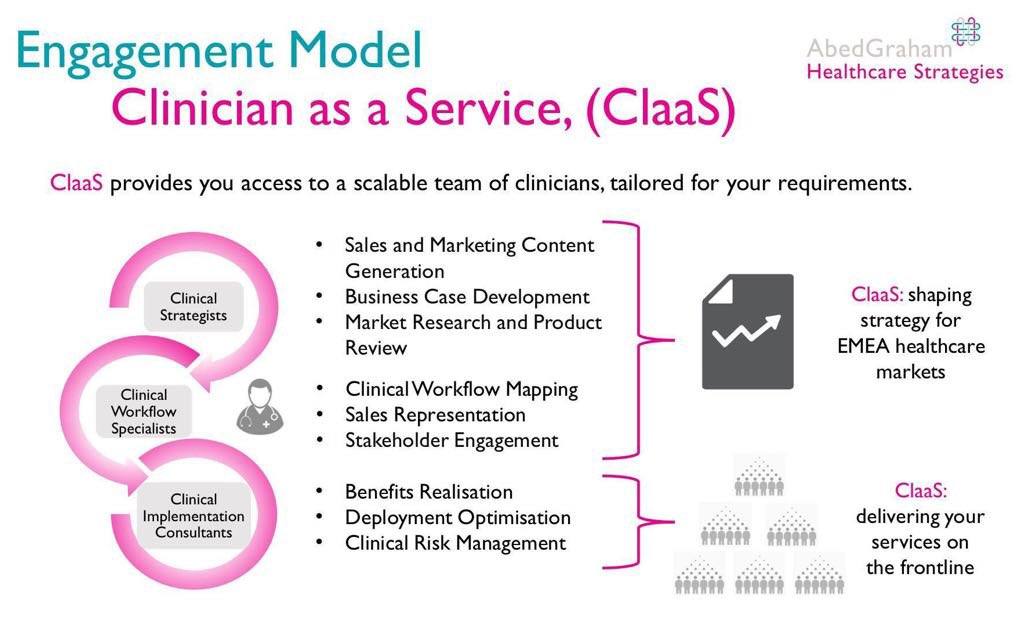
Abed says that mantra has stayed with the company and guides the tools, methods, and services the company offers and has ultimately led to its development of Clinician as a service (ClaaS). Because clinical expertise is often expensive, Abed and Graham have figured out a way to provide even small organizations and aspiring startups with access to premium expertise on a shoestring budget; AbedGraham’s quarterly fee can be up to 70% less than the cost of a single clinician.
Of course, companies big and small are now taking advantage of the service, the beauty being its scalability, so the depth and breadth of expertise offerings can grow right alongside the company. And by helping companies find their ability to develop, AbedGraham is growing, too. The company has recently expanded its ClaaS model beyond the UK through its unique franchising model, where clinicians can take charge of their own AbedGraham international hub and grow their own consultancy. The company has also recently launched a regional hub in Geneva to support France, Switzerland, and Belgium and are now actively seeking a US clinician to lead an East Coast operation.
With such a unique and intriguing business model, we at HIT Consultant sat down with Abed to learn more about his company and the importance of clinical expertise and how it can assist in tackling some of healthcare’s biggest challenges from both sides of the HIT equation: technological development and implementation.
Thanks to Abed, here’s a look at what ClaaS has to offer, the challenges of scaling a business, security issues, the promise of technologies like blockchain, AI and more:
Q
Let’s begin by talking about Clinician as a Service (ClaaS): How is this a game changer in the industry? Would it be fair to say you’re in the business of curating expertise?
ClaaS is a game-changer. We’re passionate about making clinical expertise available at scale but in a way that’s cost-effective for suppliers. A Chief Medical Officer is a significant six-figure investment, let alone having multiple sales, marketing and project management professionals on staff with clinical experience.
With ClaaS suppliers pay a set fee per quarter, that’s a lot closer to the four-figure range, which guarantees them a fixed amount of time of our clinical experts who can fulfill a variety of services from strategy to sales to project management and everything in between across all major clinical specialties. If suppliers need more then they simply ‘top-up’ the time at an agreed rate.
Now whether you would call this ‘curation,’ I’m not sure. What’s unique about AbedGraham is that we hire clinicians and train them in the AbedGraham way. We have exceptionally high standards and a range of internally developed methods that make what we do unique, which I would suggest, takes us beyond just curating clinical expertise.
Q
We know that hiring clinical experts to implement processes can be pricey, but how do your prospective clients know that ClaaS can provide them with exactly what they need?
That’s a great question. First, at a high level, you have to look at our list of clients to see that we have a track record of working with some of the most demanding and successful companies in health IT which I think speaks volumes about our diverse capabilities.
However, more specifically, we address this by having a close relationship with our clients making sure we are integrated into their operations. Before the start of any relationship, we have conversations and workshops to define our clients’ requirements and when a relationship begins we develop rolling 90-day plans to ensure that their primary needs are addressed immediately and with accountability.
Q
Can you give us an example of how it works?
One of my favorite examples of this involved an early major project we did with one of the world’s largest suppliers of cloud computing services. Their requirements were particular and involved mapping a range of clinical workflows, developing detailed clinical business cases and ultimately, compiling these into a productivity playbook that could be disseminated within their partner community.
Even before the outset of this project, we organized several meetings with the key senior stakeholders to ensure we had a clear understanding our client’s needs. We then approached this through a series of workshops with diverse stakeholders to fully flesh out the company’s approach and mission for healthcare. From there, our rolling plans and pathways to accountability meant that we could meet our client’s objectives in a way that could have a tangible impact on their business.
Ultimately, this project involved a significant part of what ClaaS would become and is an excellent example of a project whose impact we continue to see reference to this day.
Q
A service like ClaaS puts opportunity on the table for a lot of young companies trying to get their foot in the door. But where do you see this type of service giving the biggest bang for its buck? What are the biggest hurdles where clinical expertise is essential for not just success but survival?
There’s a lot to unpack there, but I’ll try to keep it concise. Typically, our clients have been large companies, but you’re right, ClaaS is accessible for smaller companies too. Regarding the most significant impact though, it varies depending on the maturity of the company, but nothing beats generating more revenue.
One of the major functions we serve is providing clinicians who can learn about a supplier’s products and can then go out in the field with a salesperson and demo a solution in a way that’s clinically relevant. They bring clinical credibility to the table but also run workflow benchmarking studies to for benefits realization purposes and write product business cases. We’ve found that businesses that make the most of this accelerate their sales cycles and close more prominent deals more consistently.
Q
Let talk about the concept of scale. It seems to be a central theme in healthcare right now and something that is at the heart of what your company offers: Whether it’s a developer trying to create a new product, or a healthcare provider working to integrate digital technologies, the concept of scalability always seems to be lurking in the background. Therefore: why has it been so difficult for companies to take their ideas from implementation into real growth and progress in healthcare?
For a long time, health IT suppliers have tried to approach clinical engagement by having a single clinician on board who they turn to for advice and expect to represent them in front of their potential customers. The problem with that approach really is that you need a diverse set of clinical experiences, and you need clinicians who are trained to fulfill distinct business functions. That can range from product development and strategy all the way through to project management and regulatory compliance. That, in our view at least, is the only way to scale in a way that’s consistently successful. There’s no point in scaling if a significant number of your customers have negative experiences. It’s unsustainable.
Q
Is the industry just too rigid for other natural forms of business development? Why do some conventional and successful business models, or even IT implementation models fail in healthcare when they do well in other industries?
Well, first and foremost, we have to remember that clinicians have not traditionally been consistently positively engaged when it comes to IT, so many are very skeptical when it comes to new health IT projects. Furthermore, clinicians are a heterogeneous group with different expectations and requirements so taking a cookie cutter approach to business development and project management is inherently more difficult. Overall though, I don’t think conventional models fail it’s just that they need to be fine-tuned to the needs of the sector rather than merely adopting a copy-paste approach. Just because it works in the world banking does not mean it will work in healthcare!
Q
Is clinical expertise the only missing ingredient here?
It’s one of the primary missing ingredients but not the only one. One of the areas we’ve specialized in at AbedGraham has been benefits realization. I think health IT suppliers often find it challenging first to build business cases for their solutions and then to prove the benefits happen over time. From clinical workflows to operational productivity and even risk and security standards, benefits realization has not been a natural area for product companies in healthcare. The reasons for this are numerous ranging from not having in-house expertise through to not willing to factor these processes in as a part of the cost of sales. However, we’ve found this to be a powerful driver for our clients when it comes to winning new business if approached correctly.
Q
Let’s tackle this idea of scale by talking about some of the more significant issues at hand in healthcare: There are some big ones, perhaps these are some of the hurdles that have made it harder to integrate IT into healthcare successfully. We’ve got a few big contenders: interoperability, security, and big data, to name a few. We could spend a lot of time on each, but for this conversation, let’s try to keep it in brief. At the heart of each issue, one could argue there is a need for clinical expertise, so with that in mind, can you share your wisdom on how those on the IT development side should be addressing these issues on behalf of their clients?
At AbedGraham, I lead our cyber security practice, and I think that’s a great area to address for your question. In the last 24 months, we’ve witnessed the increasing susceptibility of health IT solutions and healthcare providers to cyber-attacks. It’s only the tip of the iceberg, and the scope for devastating outcomes is staggering, yet many traditional cybersecurity suppliers are still not willing to invest in learning about clinical context. The butterfly effect here is that their solutions are less presentable to clinical leaders which in turn impacts the prioritization of security projects as investment areas for providers. It also means projects are less likely to be successful when procured because the suppliers are not well placed to maximize the value of their solution or demonstrate the benefits. In new areas of technology, I see this as a typical example of why health IT sub-sectors stall in their development.
Q
On the implementation side, do you have advice for health organizations when it comes to addressing these issues?
Fund, protect the time of and engage your CMIOs and CNIOs and make sure they have an executive say in the development and management of all health IT projects. Make sure you have the same expectations of health IT suppliers that they have a body of clinical expertise that can engage with yours to prepare, present, tailor and manage health IT projects from proof of concept to enterprise deployment. Hold suppliers to account by expecting them to explain their approach to benefits realization with clinical, operational, financial and governance outcomes.
Q
I want to delve into the issue of security a bit more because this is something that you speak about frequently, and I because security issues can lead both big and small companies to severe vulnerability. With all the recent ransomware attacks and security breaches, even in other industries, what can organizations be doing better to solve some of these issues: For example, what can a small, promising startup do from the development side to help improve some of these issues for its potential clients?
Understand your clients and their end-users! It’s all about people and processes. It doesn’t matter how secure your solution is at a technical level, at some point, it will fail. Whether it’s the availability of your service or its integrity, at some point, you will be compromised. What happens then? Suppliers need to be trusted partners to their customers and be well positioned to plan and execute pre-planned contingency plans in the context of preserving clinical services. A great way to do this is to appoint a Clinical Safety Officer (CSO) to complement your Chief Information Security Officer (CISO) who can run hazard workshops and clinical risk management plans relative to your solution for your customers.
Q
Similarly, what can health organizations who are integrating HIT technologies into their practices do better to protect themselves from security threats? Is there more to it than aligning themselves with the right kinds of technology?
The answer from my perspective is the same processes as the suppliers but importantly enshrine these expectations of suppliers as a part of procurement processes and hold them to account just as you would your own CISO and CSO.
Q
Just talking a little bit more in general about the cybersecurity issue: There is a lot of talk about how blockchain is going to help eliminate some of these serious risks. Do you think blockchain will be the answer the industry is looking for, why or why not? What else needs to happen for blockchain tech to tackle the problem successfully?
I’m a fan of blockchain-based applications and platforms, but at the end of the day, it’s just more technology and will not be infallible. It will not be a panacea though could, of course, be a significant advancement compared to existing systems. The focus on people and processes will be key, and for nascent technology like blockchain the sooner they start solving the people and process components as a part of pilots and proof of concepts the sooner we’ll see widespread adoption.
Q
When we talk about bringing technology from beyond the buzz to actual full-on fruition, AI seems to be the latest example of why that’s difficult in healthcare. I feel like we see this with so many technologies, especially things related to telehealth or consumer-facing technologies that are supposed to change the game. Again, are we just pulling too many carts before the horses here? Why does this keep happening? And with an example like AI in mind, how can we get one more solid path for real growth and real meaningful use?
At our Geneva office, we have an AI practice led by an Associate Partner at AbedGraham who a radiologist is. What’s interesting is that where we have seen success is in places where AI has been integrated as a part of a clinician’s workflow, so the clinicians are willing to adapt and try new ways of working. That’s great, but at the same time, I cringe every time I see an article explaining how AI will replace doctors. It’s so off-putting and is not going to motivate any clinicians to give AI the time of day when it’s so poorly positioned. The problem is hype when instead we need evidence. So, it’s the same principles – focus on context, people, and processes.
Q
I have asked quite a few questions here. So, I want to invite you to close out the conversation by telling me what you think the key and current takeaway from this conversation should be for our readers?
I’m mindful that many of your readers may know us as a European firm but what’s exciting is that this year we are expanding our services to the US starting from the East Coast. We think there’s a real passion for clinical engagement in health IT that we can support in North America and so we are actively looking for entrepreneurial clinicians interested in launching an AbedGraham America franchise. I’d love to hear from any of your readers that might be interested and would encourage them to visit our website and contact us (www.abedgraham.com).
Q
As we close our discussion, what’s your ultimate piece of wisdom you wish to share when it comes to being successful with IT in healthcare, either on the development or implementation side, or both?
It’s all about people and processes. Understand those, and you’ll do great!
