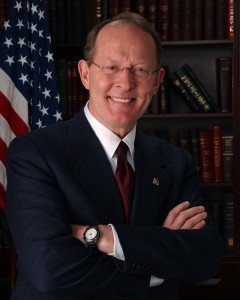
On Tuesday, U.S. Sen. Lamar Alexander (R-Tenn.) said the government should enable and encourage physicians and hospitals to adopt EHRs, rather than try to force meaningful use adoption by taking away Medicare payments.
“Transitioning to electronic health records requires a real transformation in how physicians practice medicine. They must implement pricey systems, learn how to use them, ensure their staff is trained, and pay annual licensing fees and for hardware and associated services. The administration seems to have complicated the process by rushing ahead with penalties for those who don’t adopt EHR systems.”
EHRs “should have been a really good idea,” Alexander said, but noted that half of physicians have not met the requirements of the “meaningful use” program and are now facing penalties. “A Medical Economics survey last year found nearly 70% of physicians say their EHR systems have not been worth it,” Alexander added.
The chairman’s issued the following remarks :
Health Information Technology, or Health IT, means many different things—everything from wearable gadgets that monitor your heart rate to sophisticated applications that help physicians track advancements in treatments.
Today we will be focused on Electronic Health Records (“EHRs” or “EMRs”) used by hospitals and doctors in their practices.
This committee hasn’t held a hearing on Health IT since January of 2009 – a month before the $35 billion HITECH Act became law as part of the stimulus package.
The HITECH Act was meant to unleash a new IT era where our health information would move seamlessly among doctors and hospitals to help achieve better, more coordinated care.
After the bill’s passage, doctors and hospitals rushed to join the “meaningful use” program.
Adoption rates for EHRs grew dramatically. According to the most recent data from the Center for Medicare and Medicaid Services, 48% of physicians and 59% of hospitals have at least a basic EHR system, compared to 26% and 47% in 2009.
The hope was that the program would improve care, improve coordination, and reduce costs. The evidence suggests those goals have not yet been reached.
Half of physicians have not met the requirements of the program and are now facing penalties.
A Medical Economics survey last year found nearly 70% of physicians say their EHR systems have not been worth it.
One physician surveyed wrote: “We used to see 32 patients a day with one tech, and now we struggle to see 24 patients a day with four techs. And we provide worse care.”
Doctors and hospitals have had so much difficulty meeting the Meaningful Use requirements that CMS has had to delay or change requirements three times.
So how did this happen?
Transitioning to electronic health records requires a real transformation in how physicians practice medicine.
They must implement pricey systems, learn how to use them, ensure their staff is trained, and pay annual licensing fees and for hardware and associated services.
The administration seems to have complicated the process by rushing ahead with penalties for those who don’t adopt EHR systems.
To be specific, doctors and hospitals that don’t adopt these records systems lose 1 percent of their Medicare payments in 2015. That penalty will grow to 5 percent.
To receive incentive payments, physicians and hospitals had to buy systems certified to federal government specifications. Providers assumed the certified systems would be of high quality and able to meet program requirements.
Instead, many providers discovered that certified systems have to undergo costly upgrades on short timelines to meet new requirements. Providers must pay for those upgrades, or pay even more to switch vendors.
Hospitals have spent hundreds of millions of dollars to implement and continuously upgrade their systems.
Wellmont Health System, which operates hospitals in Tennessee, went through a complete IT conversion from a one EHR system to a new one that guaranteed they’d be able to meet the requirements of the Meaningful Use Program.
Wellmont spent $125 million and expects to receive approximately $38 million in meaningful use dollars.
Wellmont is also seeing an approximately $10 million increase in annual IT costs, but hasn’t been able to calculate potential savings.
Many providers find their programs are struggling to communicate with other programs – this is called interoperability.
Children’s National Medical Center in Washington, D.C., spent $400 million on its health IT over the last four years to make a web of 138 different electronic health records systems talk to each other and work together. They received $28 million in incentive payments.
The Eye Centers of Tennessee, with five locations in East Tennessee, have spent $731,000 trying to comply with all the program requirements, but because they were not able to meet one measure, they expect a $100,000 penalty.
Enabling vs. mandating
This should have been a really good idea.
For Vanderbilt University and their patients, it has been. Vanderbilt has an award-winning program called PREDICT that includes patients’ genetic info in their medical records to help prevent unsafe administration of certain drugs. For example, that system prevented a patient in her 80s from receiving a blood thinner that she would have metabolized poorly because of her genetic variation.
Instead of government trying to make everybody do this by taking away Medicare payments, a better route would have been to find ways to enable and encourage their adoption.
But instead the administration rushed the process with its penalties—and at the same time made the federal government the arbiter of IT quality.
In 1980, I flew out to Palo Alto to meet with Steve Jobs. I had the goal of having every 8th grader in Tennessee computer literate.
We bought Macs, which were then about 4 feet tall, for every middle school in the state.
But I forgot one thing: teacher training.
It sounded like a good idea to make everyone use computers, but I should have spent more time finding ways of enabling them to use them.
That appears to be a good lesson for Washington policymakers who have rushed ahead with penalties in this program that has now created so many unhappy physicians and hospitals.
I’m interested in learning today how we can become enablers rather than mandaters.
For video of the full hearing and witness testimony, click here:http://www.help.senate.gov/
