Coordination of care, data accuracy and staff acceptance are among the top three challenges to the future use of value-based payment models, according to a new study by Availity. The study found 75 percent of providers currently participate in at least one value-based payment model in addition to traditional fee for service with 60 percent expecting them to become the dominant payment model. Despite its growing dominance, fewer than 30 percent believe they offer a good level of reward for the risk.
The Provider Attitudes Toward Value-Based Payment Models study highlights feedback from more than 500 physician practice and hospital-based professionals nationwide. It summarizes the providers’ real-world experience with these new models, revealing perspectives on the impact they will have to the health care system, and calling out the gaps and barriers hindering success. The study follows the 2013 research Availity conducted to determine the operational readiness of providers and health plans to implement value-based models of care and reimbursement.
Managing value-based payment models alongside existing fee-for-service arrangements, and across numerous health plans, is creating issues that range from accurate revenue forecasting to workflow integration challenges. According to one physician practice respondent, “The administrative complexity of administering these plans is likely to be costly. The unpredictability of the revenue stream is likely going to make administering some of these plans not worth the cost.”
Other key findings include:
– More than 60% consider themselves at least “somewhat knowledgeable” about value-based payments
– Only about 25% agree that value-based payment models make it easy to understand, track and project revenue
– More than 80% of providers cited the need for additional staff and time to manage value-based models that represent less than 20% of their current revenues
– About half agree that value-based payments models will:
– Improve population health
– Improve the patient experience
– Reduce the cost of healthcare
– Provider revenue from value-based payments is less than 20% but is expected to grow significantly over the next three years.
– More than 75% of physician practices and 88% of facilities agree that real time information sharing and access is critical for success
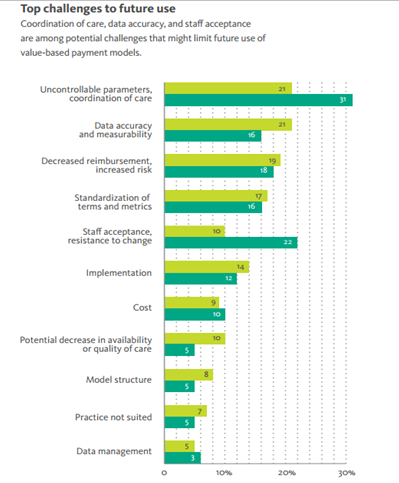
– Data accuracy, data management, and implementation assistance were cited as top gaps to value-based payment models
