Why politics, parity and performance requirements mean behavioral health hospitals should adopt now.
Imagine you go to work one day and your boss says all employees will be evaluated based on the performance of a new set of job skills that require additional training and, perhaps, new computer hardware and software. The boss also announces that some employees will be reimbursed for the cost of acquiring these skills and tools. You aren’t among this privileged group.
In government, this is called an unfunded mandate. The unlucky employee in this case is psychiatric hospitals, who aren’t eligible for Meaningful Use incentives even while Congress and the Obama administration have legislated greater accountability:
- A precursor to the 2010 Affordable Care Act (ACA), the Mental Health Parity and Addiction Equity Act of 2008 mandated that insurers must make the financial cost of benefits—co-pays, deductibles, out-of-pocket maximums—equal for psychiatric and physical care.
- By making behavioral health an Essential Health Benefit, the ACA requires health plans to cover mental health on par with other types of care.
- On October 1, 2012, CMS launched the Inpatient Psychiatric Facility Quality Reporting Program (IPFQR), a pay-for-reporting program in which facilities could lose federal dollars by not providing data on Hospital Based Inpatient Psychiatric Services (HBIPS):
- Screening for violence risk, psycho trauma Hx, patient strengths
- Hours of physical restraint use
- Hours of seclusion use
- Patients discharged on multiple antipsychotic medications
- Patients discharged on multiple antipsychotic medications with appropriate justification
- Post discharge continuing care plan created
- Post discharge continuing care plan transmitted to next level of care provider upon discharge
Whether explicit or implicit, these programs amount to unfunded EHR mandates. How so?
Organizations still on paper records will find it expensive and inefficient to capture events and collect results for both reporting to government and submitting claims to insurance companies. Hospitals will need to train clinicians to document post-discharge continuity of care plans. They will have to train staff to send plans by snail mail or fax to the provider at the next level. Then they will also need to do chart reviews to assure that all these steps took place and the data is recorded in a spreadsheet or database. Any quality improvement process that requires benchmarking and scoreboarding of performance based on these measures will be a tremendous challenge using paper records.
For acute care hospitals, Meaningful Use Stage 2 requires standardized documentation, time-date capture of events, data analytics and reporting, and transmitting the patient’s care plan to the next-level provider upon discharge; documentation and transmission are also built into the requirements. Good EHRs support the attestation, benchmarking and scoreboarding that drive improvement on performance criteria. So why is the goal of better care through rigorous reporting only valid for acute care hospitals?
The question becomes more relevant when it is about actual lives instead of arcane policy.
We’re all familiar with the horrific events associated with the mental health of individual citizens. Sandy Hook, Aurora, Fort Hood and Columbine are no longer just places—they are also shorthand for societal issues we can’t get a handle on. They are political flashpoints for arguments about whether the real issue is guns or the disturbed individuals who carried them.
Congressman Tim Murphy (R-PA) is working to change one side of that equation. Champion of the Helping Families Mental Health Crisis Act (72 bipartisan sponsors) and the only practicing psychologist in Congress, Murphy represents a district in which 19 students at Franklin Regional High School were stabbed by a classmate. A confrontational phone call the troubled young man had the night before suggests that active intervention may have prevented the assaults.
“These (the phone call) are sparks, but there’s usually a long fuse that goes with that,” Murphy said.
The Helping Families act provides for more acute psychiatric beds and better access to care; most importantly, it also encourages a shift in the standard for committing someone for treatment from “posing a danger to themselves or someone else” to “need for treatment.” The legislation enables intervention before absolute proof of danger to self or others is manifest.
To do this, psychiatric hospitals need more support. While roughly 85 percent (~4,600) of acute care hospitals have adopted and attested for MU, a mere 2 percent of behavioral health hospitals have adopted EHRs. About 30 percent cite upfront costs as the prohibitive barrier. So while CMS and the ONC mandate and incent EHR adoption for everyone else, they exclude behavioral hospitals to the detriment of society as a whole.
In America, we generally demonstrate our seriousness about an issue by investing in a sound solution. It’s time to invest seriously in mental health treatment for all Americans that need it, and EHR support for that care is an essential first step.
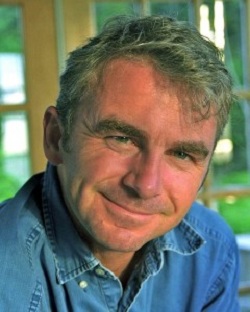
Edmund Billings, MD, is chief medical officer of Medsphere Systems Corporation, the developer of the OpenVista electronic health record.