What You Should Know:
– Inovalon, a provider of data-driven healthcare solutions, has announced an expanded collaboration with Amazon Web Services (AWS) to enhance its Converged Record Review™ solution.
– The enhancement is in direct response to the new Centers for Medicare & Medicaid Services (CMS) requirement for annual Risk Adjustment Data Validation (RADV) audits for all Medicare Advantage (MA) contracts, beginning in 2026.
Increasing Scrutiny from Health Plans
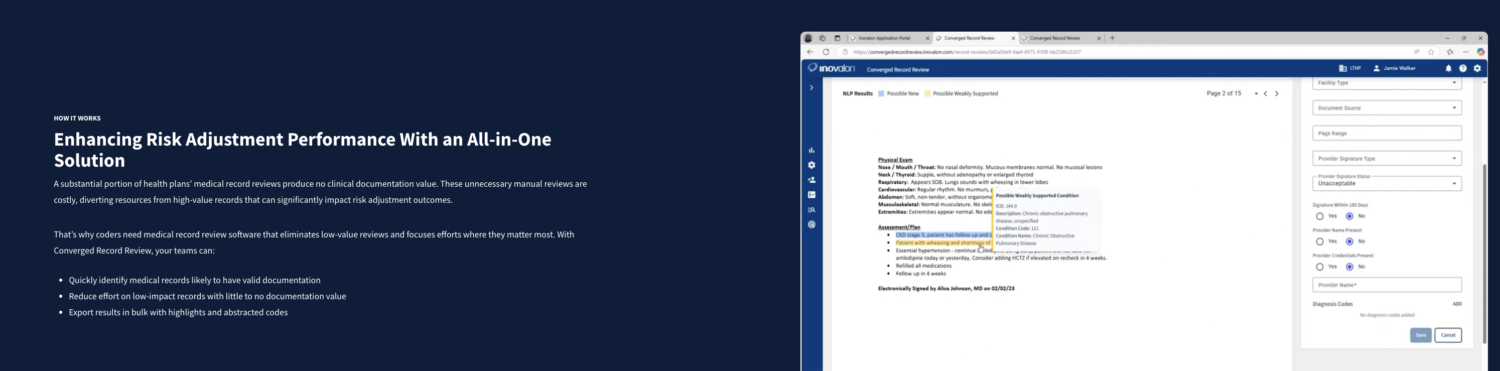
Health plans are facing increased scrutiny regarding their clinical support for submitted diagnoses. Without a way to manage this, they face operational burdens, potential damage to their reputation, and additional financial risks from payment recoupment if claims are not sufficiently supported. The Converged Record Review solution, powered in part by Amazon Comprehend Medical’s natural language processing (NLP) and machine learning (ML) capabilities, helps MA plans proactively prepare for these audits.
Streamlining Audit Preparation with AI and Analytics
The enhanced solution assists MA plans in several key areas to prepare for RADV audits:
- It enables the rapid evaluation of potential documentation gaps to reduce audit risk.
- It integrates with Inovalon’s
Converged Risk Surveillance Analytics™ to proactively identify and remove diagnoses that are not supported. - It streamlines chart reviews and validates diagnoses during audits by surfacing the most clinically relevant information from medical records.
These combined capabilities help health plans with both Hierarchical Condition Category surveillance and retrospective audit support, which are critical for RADV preparedness. This helps to improve the accuracy of risk scores and ensure accurate reimbursements.
Michael Jones, President of Inovalon’s Payer Business Unit, stated that CMS is “raising the bar on RADV audit expectations” and that Medicare Advantage plans “must act quickly to prepare for 2026”. He noted that the expanded collaboration with AWS provides health plan customers with the necessary “intelligence, infrastructure, and confidence they need to safeguard revenue and maintain compliance”.
