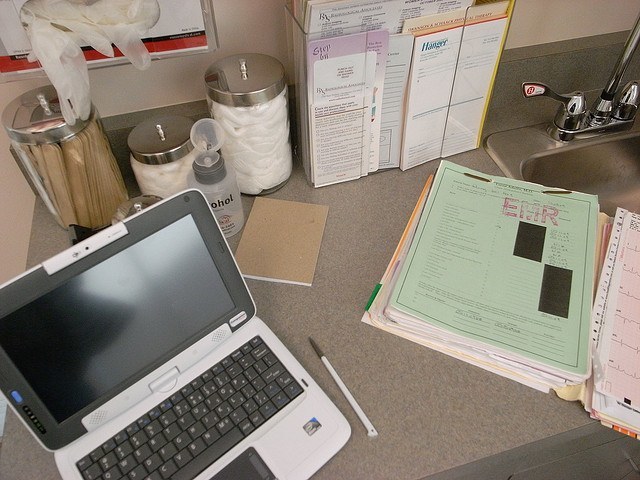
By the year 2024, the U.S. Department of Health and Human Services wants interoperability between disparate electronic health records systems (EHRs) to be a common capability. This would allow patient data to be shared among authorized practitioners more seamlessly. But how do patients feel about this?
According to a recent survey conducted by Software Advice, 46 percent of patients want their doctors to directly exchange the health records, and fewer (21 percent) favor in-person delivery. When asked how their medical records are shared among multiple providers, only 39 percent of patients say providers directly exchange records, while 25 percent must deliver a paper copy to the other provider themselves. The findings illustrate the challenges patients faced when trying to obtain and share their medical records between multiple providers.
Despite the rapid increase in EHR adoption, the real issue preventing direct helath data exchanges between providers is that many EHR systems are unable to interface with each other, let alone exchange patient information in an efficient way.
Here are some four factors why Software Advice believes EHR interoperability has been such a challenge:
1. Resistance from some vendors: Politicians, medical associations and physicians are concerned about some vendors who they say engage in “information blocking”—that is, purposely keeping patient health information “locked” into a system, in order to later charge data exchange fees.
2. Prohibitively high data exchange fees: In some cases, it is possible for an EHR system to send and receive patient information from other systems. However, some vendors reportedly charge $5,000 to $50,000 to set up such connections.
3. Lack of incentives to develop interoperability: Vendors haven’t been sufficiently incentivized to make EHR interoperability a key capability, which is why its development has lagged, according to this recent study.
4. Technical variations: There are literally hundreds of EHR products out there with different technology architectures, service models and capabilities. This makes it hard to create one standard format for sharing data.
For more information, the full report can be found here
