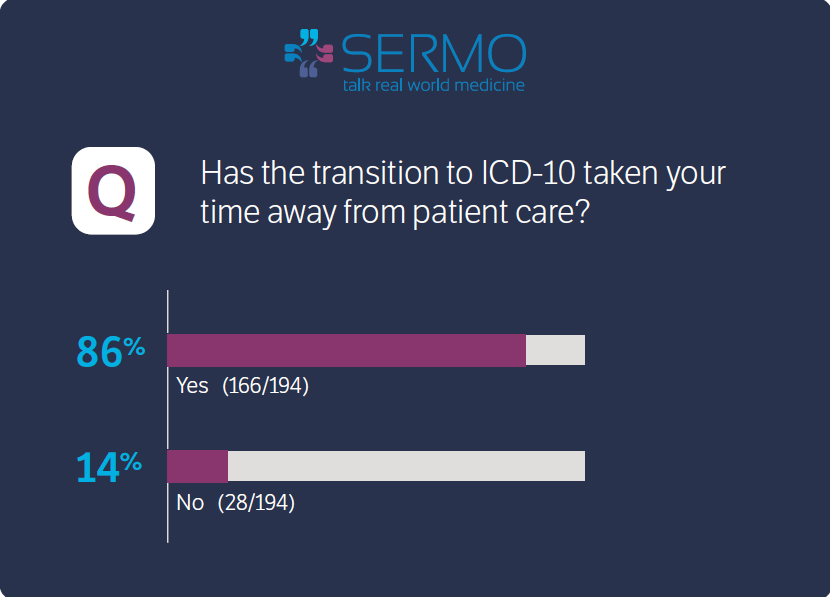
It’s been a full week since the ICD-10 compliance date took effect on 10/1. So how do doctors feel about patient care impact of ICD-10? SERMO, a social media network exclusively for doctors, asked members if the transition is taking their time away from patient care and the numbers overwhelmingly showed that it is. Out of nearly 200 members who responded to the poll, 86% stated it has impacted patient care while only 14% said it has not.
Here are some more insights provided by some of the doctors about their recent ICD-10 transition experience after one week:
Primary Care Provider:
“It has added boatloads of time.
1. We are not able to do referrals because the online referral system will not accept ICD10 codes (for our biggest payer).
2. Wait times to get thru to insurance company now is hours (3 hours is not unusual)
3. The personnel at the insurance companies do not know how to answer any ICD10 related questions: the answer is, submit and we will see.
4. We were locked off the sites of several of our payers because they were updating
5. Our local Medicare carrier closed for the last week because of technical difficulties
6. And now the wait game to see if we will be paid
7. and when all that is ironed out, I expect the 3rd parties and government to reduce our reimbursements using ICD10 and citing quality measures (which they will set to maximize their own profits).
8. I used to enter my own charges. I quit on October 1st and now my biller is doing it. I used to bill every day…..we are now 3 days behind.
9. It takes a gazillion of hours to fill out the lab requisition forms looking up new and useless codes. and on and on and on….and no one is listening……”
Pediatrician
“I recently saw a young man as a follow up from a car accident. Under the old ICD 9 I would type motor vehicle, and get the choices, passenger and driver. With the ICD 10, I typed motor vehicle, the first 20 choices were 3 wheeled vehicles and all different descriptions. I took a couple of minutes to find the right code. All the time taken from the patient. I real waste and no improvement in quality of care.”
Family Medicine
“Right now it’s about an extra 60-80 minutes per 12 hour ER shift. Each diagnosis that used to be in the chart from past encounters can’t be ‘checked off’, it has to be re-translated to ICD-10 by the person making the first post 10/1 encounter, which for the next few months will oftentimes be the ER physician. 2-3 sets of multiply nested boxes to filter through per patient, 15-30 times a shift…”
Allergy and Immunology
“ICD-10 is one more impediment to good medicine for the patient. It wastes too much time, decreasing the number of patients I can see a day. I am now having to schedule some return visits farther out than is ideal as a result. Waiting time for new patient appointments is longer.”
So, how has week 1 fared for you? Let us know.
Featured image credit: cesarastudillo via cc
